Abstracts
OBJECTIVE: To determine whether a biopsy of the synovia of the carpal tunnel is able to identify systemic diseases that were not diagnosed by clinical examination and laboratory tests. METHODS: Anatomical pathology P examinations of synovial tissue were performed in 46 patients that underwent open carpal tunnel release. Anatomical pathology examination with hematoxylin-eosin staining determined the intensity of the inflammatory process and the authors proposed a new classification of the injury according to the intensity of the inflammatory process. RESULTS: The anatomical pathology examination showed that 56.6% were classified as grade I (unchanged inflammation), 32.6%, grade II (leukocyte infiltration and discreetmoderate fibrosis), 4.3%, grade III (leukocyte infiltrate and intense fibrosis, the presence of fibrin and vascular neoformation) and 6.5%, grade IV (changes described above associated with the presence of local calcification and giant cells). Two patients with amyloidosis were classified as grade I and II and no stockpiles of amyloid material were found on their slides. Two patients with hyperparathyroidism and another with chronic kidney failure were classified as grade IV. CONCLUSION: Synovial biopsy of the carpal tunnel did not make early diagnosis of potential systemic diseases possiblein patients with carpal tunnel syndrome, and adds extra costs to the procedure.
Carpal tunnel syndrome; Biopsy; Nerve crush
OBJETIVO: Verificar se a biópsia da sinóvia do túnel do carpo é capaz de identificar patologias sistêmicas que não foram diagnosticadas clinicamente ou por exames laboratoriais. MÉTODO: 46 exames anatomopatológicos da sinóvia dos tendões flexores no túnel do carpo de pacientes submetidos à liberação aberta para o tratamento desta síndrome compressiva foram, retrospectivamente, analisados. Os autores propuseram uma nova classificação para a lesão de acordo com a intensidade do processo inflamatório. RESULTADOS: O exame anatomopatológico mostrou que 56,6% das lâminas foram classificadas como grau I (sem alterações inflamatórias), 32,6%, grau II (infiltrado leucocitário e fibrose discretos, além de hialinose), 4,3%, grau III (infiltrado leucocitário e fibrose intensos, presença de fibrina e neoformação vascular) e 6,5%, grau IV (as alterações acima descritas associadas à presença de calcificação local e células gigantes). Dois pacientes com amiloidose foram classificados como graus I e II e não foram encontrados depósitos de material amilóide em suas lâminas. Dois pacientes portadores de hiperparatireoidismo e outro com insuficiência renal crônica foram classificados como grau IV. CONCLUSÃO: A realização da biópsia da sinóvia do túnel do carpo, além de agregar custos adicionais ao procedimento, não possibilitou o diagnóstico precoce de doenças sistêmicas em pacientes portadores de síndrome do túnel do carpo.
Síndrome do túnel carpal; Biópsia; Compressão nervosa
ORIGINAL ARTICLE
Orthopedics and Traumatology Service of Hospital Felício Rocho (Belo Horizonte - MG)
Mailing Address
ABSTRACT
OBJECTIVE: To determine whether a biopsy of the synovia of the carpal tunnel is able to identify systemic diseases that were not diagnosed by clinical examination and laboratory tests.
METHODS: Anatomical pathology P examinations of synovial tissue were performed in 46 patients that underwent open carpal tunnel release. Anatomical pathology examination with hematoxylin-eosin staining determined the intensity of the inflammatory process and the authors proposed a new classification of the injury according to the intensity of the inflammatory process.
RESULTS: The anatomical pathology examination showed that 56.6% were classified as grade I (unchanged inflammation), 32.6%, grade II (leukocyte infiltration and moderate fibrosis), 4.3%, grade III (leukocyte infiltrate and intense fibrosis, the presence of fibrin and vascular neoformation) and 6.5%, grade IV (changes described above associated with the presence of local calcification and giant cells). Two patients with amyloidosis were classified as grade I and II and no stockpiles of amyloid material were found on their slides. Two patients with hyperparathyroidism and another with chronic kidney failure were classified as grade IV.
CONCLUSION: Synovial biopsy of the carpal tunnel did not make early diagnosis of potential systemic diseases in patients with carpal tunnel syndrome, and adds extra costs to the procedure.
Keywords: Carpal tunnel syndrome. Biopsy. Nerve crush.
INTRODUCTION
Carpal Tunnel Syndrome (CTS) results from compression of the median nerve inside the carpal channel.
Paget1 described compression of the median nerve in the carpal tunnel after trauma. Marie and Foix2 described the histopathology of carpal tunnel syndrome, correlating it with mechanical compression of the median nerve. Learmonth3 performed the first decompressive surgery. Phalen4 described a test for evaluation of median nerve compression. Semple and Cargil5 compared the results of several types of surgical incisions, concluding that there is no influence in terms of results, excepting with transversal incisions. Sunderland6 described the physiopathology of carpal tunnel syndrome, in which he attributed to the initial lesion an intrafunicular anoxia caused by obstruction of the intraneural venous return, produced by a pressure increase in the carpal tunnel of any nature.
Carpal tunnel syndrome occurs more frequently in patients between 40 and 60 years of age, and is more common among women.7-9 Any condition that increases the content or that decreases the continent of the carpal tunnel may start off the symptoms. Among the systemic conditions that can lead to CTS, we emphasize rheumatoid arthritis, kidney failure, hypothyroidism, diabetes mellitus, amyloidosis, pregnancy, Raynaud's phenomenon and obesity. Local causes such as Colles' fracture, edema resulting from trauma or infection and tumors,10 are among the agents that trigger the disease. CTS can also be associated with De Quervain's tenosynovitis, rhizarthrosis and trigger finger.
Paresthesia in the median nerve territory is the most frequent syndrome, and in more severe cases, wakes the patient up during the night. The clinical diagnosis is confirmed by the compression test of the examiner's thumb on the topography of the carpal tunnel11 and by Tinel's12 and Phalen's4 signs. The elevation test of the affected upper limb, insufflating the sphygmomanometer cuff on the arm between systolic and diastolic pressures, reproduces the symptoms. Atrophy of the thenar eminence is present in the more severe and long-lasting cases. It is considered that electroneuromiography presents sensibility of 90% and specificity of 60%.13 Ultrasonography, magnetic resonance and computed tomography are imaging exams reserved for cases in which the etiology arises from an expansive process.
The treatment of CTS should be based on its etiology. Local factors should be removed and systemic factors, corrected.
Patients with slight symptoms respond well to non-surgical measures such as non-hormonal anti-inflammatory drugs (NHAI), physiotherapy and orthosis. Some authors advocate the local infiltration of corticosteroids in cases in which thenar eminence does not present atrophy. Clinical intractability leads to the need for surgical treatment, which can be open or endoscopic.14-20 Anterior displacement of the median nerve, its adherence to the transverse carpal ligament and reflex sympathetic dystrophy are some of the possible complications of surgical treatment.21
The aim of this study is to evaluate the need to perform routine anatomopathological examination on patients with CTS and to analyze the impact of biopsy performance on the cost of the procedure.
MATERIAL AND METHOD
During the period from January 1996 to November 2002 forty-six surgeries were performed for CTS treatment in our service. The surgical option was by the open route, with "L" shaped ulnar access22 (Figure 1), executing the opening of the transverse carpal ligament, external epineurotomy of the median nerve and biopsy of the synovia of the carpal tunnel. All the procedures were performed by the same surgeon.
The results of the anatomopathological exams were analyzed and classified according to the intensity of the inflammatory process, following the classification proposed by the authors. The slide staining method was with hematoxylin-eosin. This classification involves:
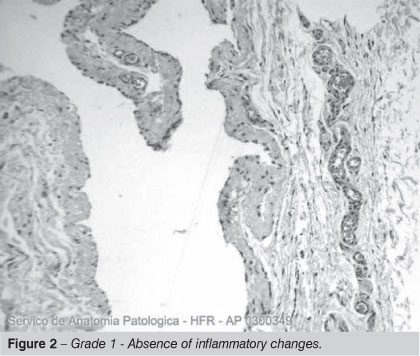
Grade I: unchanged inflammation. (Figure 2)
Grade II: modest leukocyte infiltrate and fibrosis, besides hyalinosis
Grade III: intense leukocyte infiltrate and fibrosis, presence of fibrin and vascular neoformation. (Figure 4)
Grade IV: the alterations described above associated with the presence of local calcification and giant cells. (Figure 5)
The study was approved by the Committee of Ethics in Research of our institution.
RESULTS
Distribution by gender was 86.9% for females and 13.1% for males. The right side was affected in 64.5% and the left, in 35.5%. Age ranged from 21 to 86 years, with mean age of 51 years.
In the anatomopathological evaluation, 56.6% of the slides were classified as grade I, 32.6% as grade II, 4.3% as grade III and 6.5%, as grade IV. (Figure 6)
Two patients with amyloidosis were categorized in grades I and II and no deposition of amyloid material was found on the slides of these patients. Two patients that presented hyperparathyroidism and another with chronic kidney failure were classified as grade IV.
DISCUSSION
Surgical indication was based on clinical intractability and on the exclusion of corrigible systemic causes that could cause compressive symptoms.
The anatomopathological examination of the synovia of the carpal tunnel of patients treated surgically was performed as routine. The goal was to identify at an early stage pathologies not diagnosed clinically or by laboratory exams.
All the patients operated in the six-year period were included in the study and their distribution in relation to gender, age and affected side was similar to that found in literature.7-9
The route of access used for the performance of the surgery was the "L" shaped ulnar access,22 modification of the route proposed by Tubiana,23 which crosses the palmar crease in a zigzag pattern.
An anatomopathological classification of the synovial tissue of the carpal tunnel was used to facilitate the analysis of the biopsy results, based on the intensity of the local inflammatory process. Grade I represents the absence of inflammatory alterations. Grade II shows discrete leukocyte infiltrate and fibrosis, besides hyalinosis. At grade III, there are intense fibrosis and leukocyte infiltrate, besides vascular neoformation. At grade IV, besides the lesions described, the presence of local calcification and giant cells is also observed.
Most of the patients (56.6%) did not present inflammatory process in the synovial tissue (grade I). Leukocyte infiltrate was observed in 43.4%. Patients with known diagnosis of hyperparathyroidism showed the presence of mononuclear inflammatory infiltrate, multinuclear giant cells and calcification focuses, characterizing moderate chronic synovitis, and were classified as grade IV. The same finding was observed in individuals with chronic kidney failure.
In the patients with amyloidosis, the presence of amyloid deposits was not observed on the slides. One of the patients did not present inflammatory infiltrate (grade I) and another, slight inflammatory infiltrate (grade II).
Schuind et al.24 classified lesion of the synovial tissue of the carpal tunnel at three levels, according to the intensity of fibrosis and the presence of zones of necrosis. In his series, which consisted of 34 samples, it was observed that 50% of the patients presented fibrous hypertrophy with localized areas of necrosis.
Our microscopic findings, observed with the same stain (hematoxylin-eosin - HE), did not demonstrate areas of necrosis. We verified the presence of leukocyte infiltrate and, in some cases, vascular neoformation, which was not observed by Schuind et al.24 Due to these observations, it was not possible to correlate our findings with the classification proposed by Schuind et al.24 which prompted us to create a new classification.
No early diagnosis was obtained of systemic diseases not diagnosed clinically or by laboratory exams, through anatomopathological findings of synovial tissue of the carpal tunnel, which authorizes us to not perform the exam as routine.
Analyzing the treatment cost, excluding medical fees, an increase of around 10% was verified in performing the simulation of procedures carried out with synovial tissue biopsy in relation to those performed without biopsy.
CONCLUSION
We concluded that the performance of biopsy as routine is not necessary in patients undergoing surgical treatment for compressive carpal tunnel syndrome. Biopsy performance implies additional costs to the procedure and does not produce benefits in relation to the early diagnosis of systemic pathologies.
REFERENCES
- 1. Paget J. Lectures on Surgycal Pathology. Philadelphia: Lindsay & Blakston; 1854. p. 42.
- 2. Marie P, Foix C. Atrophie isolée de l'eminence thénar d'origine névritique: role du ligament annulaire anterieur du carpe dans la pathogénie de la lésions. Rev Neurol. 1913;26:647-9.
- 3. Learmonth JR. The principle of descompression in the tratament of certain diseases of peripheral nerves. Surg Clin North Am. 1933;13:905-13.
- 4. Phalen GS. Spontaneous compression of the median nerve at the wrist. J Am Med Assoc. 1951;145:1128-33.
- 5. Semple JC, Cargil AO. Carpal tunnell syndrome: results of surgical descompression. Lancet. 1969;1:918-9.
- 6. Sunderland S. The nerve lesion in the carpal tunnel syndrome. J Neurol Neurosurg. 1976;39:615-26.
- 7. Barbieri CH, Cisneros RR, Audi Filho A. Síndrome do túnel do carpo. Rev Bras Ortop. 1985;20:255-60.
- 8. Sobania LC, Macohin GSG. Síndrome do túnel carpiano. Rev Bras Ortop. 1998;23:175-82.
- 9. Pardini Junior AG, Maciel Filho DF, Rodrigues VG. Síndrome do túnel do carpo. Rev Bras Ortop. 1974;9:227-31.
- 10. Chambriard C, Fernandes S, Osório L, Couto P. Síndrome do túnel do carpo devido à calcinose tumoral. Rev Bras Ortop. 1993;28:694-6.
- 11. Durkan JA. A new diagnostic test for carpal tunnel syndrome. J Bone Joint Surg Am. 1991;73:535-8.
- 12. Tinel J. Nerve wound: symptomatology of peripheral nerve lesion caused by war wounds. New York: Wiiliam Wood; 1918. p. 34-6.
- 13. Wright PE. Carpal tunnel, ulnar tunnel, and stenosing tenosynivitis. In: Canale ST, Beaty JH, editors. Campbell's operative orthopaedics. Philadelphia: Mosby; 2003. p. 3762.
- 14. Severo A, Aysemberg H, Pitágoras T, Nicolodi D, Mentz L, Lech O. Análise de 146 casos operados pela miniincisão. Rev Bras Ortop. 2001;36:330-5.
- 15. Pignataro MB, Ruschel PH, Folberg CR, Carneiro RS. Técnica de liberação do túnel do carpo com mini-incisão palmar e uso do retinaculótomo. Rev Bras Ortop. 1998;33:190-4.
- 16. Fernandes CH, Meirelles LM, Carneiro RS, Faloppa F, Albertoni, WM. Tratamento da síndrome do túnel do carpo por incisão palmar e utilização do instrumento de Paine. Rev Bras Ortop. 1999;34:260-70.
- 17. Paine KWE, Polyidisk KS. Carpal tunnel sindromy: descompression using the Paine retinacuotome. J Neurosurg. 1983;59:1031-6.
- 18. Cortez M, Costi LE, Machado GS, Ribeiro FGL, Silva PFS. Liberação endoscópica do túnel do carpo pela técnica de Agee com instrumental modificado. Rev Bras Ortop. 1997;32:75-8.
- 19. Mattar Junior R, Starck R, Azze RJ, Camilo AC. Liberação endoscópica do túnel do carpo por acesso único: estudo comparativo com a técnica aberta convencional. Rev Bras Ortop. 1996;31:297-302.
- 20. Zumiotti AV, Ohno PE. Tratamento cirúrgico da síndrome do túnel do carpo por via endoscópica. Rev Bras Ortop. 1994;29: 561-4.
- 21. Zumiotti AV, Ohno PE, Prada FS, Azze RJ. Complicações do tratamento cirúrgico da síndrome do túnel do carpo. Rev Bras Ortop. 1996;31:199-202.
- 22. Galbiati JA, Komatsu S, Faloppa F, Albertoni WM, Silva SEAB. Via de acesso ulnal na síndrome do túnel do carpo. Rev Bras Ortop. 1991;26:389-94.
- 23. Tubiana R. [Surgical approach to the carpal tunnel]. Ann Chir Main. 1986;5:85-7.
- 24. Schuind F, Ventura M, Pasteels JL. Idiopathic carpal tunnel syndrome: histologic study of flexor tendon synovium. J Hand Surg Br. 1990;29:325-8.
Pathological study of the synovial tissue of patients who underwent open carpal tunnel release
Publication Dates
-
Publication in this collection
09 Aug 2010 -
Date of issue
2010
History
-
Received
10 May 2009 -
Accepted
25 Oct 2009