Abstract
Introduction
Temporoamndiular Disorders (TMD) involve the masticatory muscles, temporomandibular joint (TMJ) or both. The most common symptom is pain, which is usually located in the muscles of mastication, pre-auricular region, and / or ATM, especially during mandibular function. The main treatment for TMD is related to pain relief.
Objective
The purpose of this case report was to evaluate the reduction of pain symptoms using Visual Analogue Scale (VAS) of patients with TMD treated with counseling and use of occlusal splint (OS).
Material and method
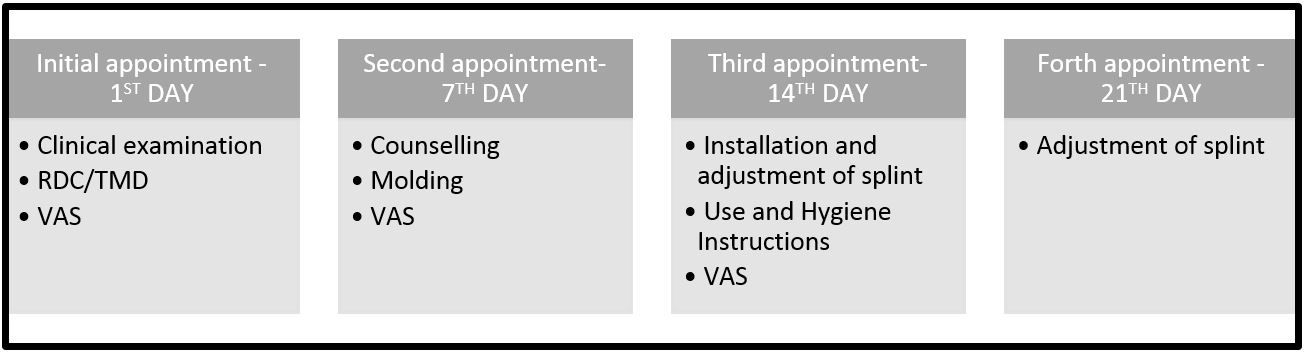
16 subjects had participated in this study, that was composed by 4 appointment with 7-day interval between each (CEP FOP / Unicamp – 137/2009). In the first, an examiner used the Research Diagnostic Criteria for Temporomandibular Disorders (RDC / TMD) to diagnose each patient and delivered a VAS to register the intensity of daily pain. In the second, counseling, molding of both dental arcs to fabricate the OS and the delivery of new VAS were performed. In the third, there was the installation and adjustment of the OS and the delivery of another scale, and in the last, possible adjustments on the OS were done. Data were analyzed by ANOVA two way and Tukey post-test at 5% significance level.
Result
There was significant difference when comparing the intensity of pain of individuals after installation of splint with the baseline data and after counseling (p = 0.05).
Conclusion
According to the result of this study, the treatment of TMD associating counseling occlusal splint is effective in reducing pain intensity.
Descriptors:
Temporomandibular joint disorders; counseling; pain measurement; myofascial pain; occlusal splint
Resumo
Introdução
As desordens temporomandibulares (DTM) envolvem a musculatura mastigatória, as articulações temporomandibulares (ATM) ou ambas. O sintoma mais frequente é a dor, geralmente localizada nos músculos da mastigação, na região pré-auricular, e/ou na ATM, principalmente durante as funções mandibulares. O tratamento principal para pacientes com DTM consiste no alívio da dor.
Objetivo
O objetivo deste estudo de relato de casos foi avaliar a redução da sintomatologia dolorosa, utilizando Escala Visual Analógica (EVA), de pacientes com DTM por meio do aconselhamento e utilização de dispositivos interoclusais (DI).
Material e método
Um total de 16 indivíduos participaram deste estudo, composto de 4 consultas com intervalo de 7 dias entre cada uma delas (CEP FOP/Unicamp – 137/2009). Na primeira consulta, foi realizado o diagnóstico através do questionário para diagnóstico de DTM, o Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) e entregue a EVA para registrar a intensidade de dor diária. Na segunda consulta, foi realizado o aconselhamento, moldagem para confecção dos DI e a entrega de nova EVA. Na terceira, houve a instalação e ajuste dos DI e a entrega de outra escala, e na última, realização de possíveis ajustes dos DI. Os dados foram analisados por meio do ANOVA a 2 critérios e utilizado o pós-teste de Tukey, com nível de significância de 5%.
Resultado
Observou-se diferença significante quando se comparou a intensidade de dor dos indivíduos após instalação dos DI com as informações inicias da pesquisa e após o aconselhamento (p=0,05).
Conclusão
A partir dos dados obtidos, pode-se concluir que o tratamento de DTM por meio do DI, seguido do aconselhamento, é eficaz na redução da intensidade da dor.
Descritores:
Disfunção temporomandibular; aconselhamento; medição da dor; dor orofacial; placas oclusais
INTRODUCTION
Orofacial pain is the main symptom of Temporomandibular Disorder (TMD), which motivates the patient to seek treatment. The painful symptomology, which ranges from sensitivity or discomfort to the worst pain possible, may affect the quality of life of the patient on different levels. It may interfere with activities of daily living, work performance, and reduce the quality of sleep, among others.
TMD is a collective expression, which involves a series of clinical signs and symptoms that affect the masticatory musculature, temporomandibular joint and associated structures11 Sipilä K, Suominen AL, Alanen P, Heliövaara M, Tiittanen P, Könönen M. Association of clinical findings of temporomandibular disorders (TMD) with self-reported musculoskeletal pains. Eur J Pain. 2011 Nov;15(10):1061-7. http://dx.doi.org/10.1016/j.ejpain.2011.05.001. PMid:21664847.
http://dx.doi.org/10.1016/j.ejpain.2011....
. There are several treatment possibilities for patients with this disorder, which may be conservative or invasive, found in the literature. Treatment for TMD is not standardized due to the different etiologies and the distinct structures that might be affected.
Treatment for TMD aims for the elimination or remission of the pain and the reestablishment of normal functions. Occlusal Splints (OS) are widely used to treat patients with TMD, with the aim of stabilizing the occlusion, reorganizing the function of the TMJ and masticatory muscles and reducing or eliminating the painful symptoms22 Nelson SJ. Principles of stabilization bite splint therapy. Dent Clin North Am. 1995 Apr;39(2):403-21. PMid:7781834.. They are also indicated for patients with bruxism, especially sleep bruxism, to prevent wear or fractures to the teeth33 Boero RP. The physiology of splint therapy: a literature review. Angle Orthod. 1989;59(3):165-80. PMid:2672904.. In addition to the OS, counseling therapy (CT), consisting of explaining the etiology, the patient’s current condition and new habits, have been used in the treatment of TMD. Whether combined with other therapies or isolated, CT has obtained favorable results in the control of pain44 Michelotti A, Iodice G, Vollaro S, Steenks MH, Farella M. Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles. J Am Dent Assoc. 2012 Jan;143(1):47-53. http://dx.doi.org/10.14219/jada.archive.2012.0018. PMid:22207667.
http://dx.doi.org/10.14219/jada.archive....
5 Alencar F Jr, Becker A. Evaluation of different occlusal splints and counselling in the management of myofascial pain dysfunction. J Oral Rehabil. 2009 Feb;36(2):79-85. http://dx.doi.org/10.1111/j.1365-2842.2008.01913.x. PMid:18976268.
http://dx.doi.org/10.1111/j.1365-2842.20...
-66 Truelove E, Huggins KH, Mancl L, Dworkin SF. The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: a randomized controlled trial. J Am Dent Assoc. 2006 Aug;137(8):1099-107, quiz 1169. http://dx.doi.org/10.14219/jada.archive.2006.0348. PMid:16873325.
http://dx.doi.org/10.14219/jada.archive....
.
Based on the information above, the objective of the present study was to evaluate the reduction of painful symptomology using the Visual Analog Scale (VAS) in patients with TMD, through counseling and using the OS.
Case Report
In the present study, patients with orofacial pain who sought dental services at the outpatient center of the College of Dentistry of Piracicaba, Unicamp, were treated. Individuals were excluded from this report who required treatment for caries and/or periodontal disease, whose pain could interfere with the data analysis; minors under 18 years of age; patients with previous experience or currently using OS and those who did not show up regularly for treatment, did not use the OS regularly or who required associated pharmacological therapy during the period of the study. The final sample totaled 16 patients.
The present study was approved by the Committee for Ethics in Research of the Piracicaba Dental School/Unicamp (protocol no. 137/2009). All patients signed the Free and Informed Consent form. The treatment chosen was based on the conservative treatment protocol, consisting of: diagnostic appointment, counseling and molding appointment, installation of the intraoral splint and occlusal adjustment appointment, and follow up appointment, as illustrated in Figure 1.
At the first appointment, the Research Diagnostic Criteria for Temporomandibular Disorder (RDC/TMD) were applied so that a final diagnosis could be made Group I – Muscular Disorders; Group II – Dislocated Disks; Group III - arthralgia, osteoarthritis, osteoarthrosis. A single, calibrated examiner was responsible for implementing and verifying the RDC/TMD. At the end of this appointment, the patient received a VAS to record the pain intensity daily. The VAS was a 100-millimeter straight line, on which there were 2 reference points: at the beginning, identified as “No pain” and at the end, identified as “Worst pain possible”. The patient was instructed to draw a vertical line on this line between these reference points, to correspond to the quantitative assessment of the pain sensation. Using a millimetered ruler, the initial point of the scale (absence of pain) and the mark made by the patient were measured. The patients were also instructed not to take any pain medication during the entire study and, if they did, they should register the day and the name of the drug on the VAS.
After 7 days, the patient returned to deliver the VAS and begun counseling therapy. This procedure consisted of informing the patient of the diagnosis obtained with the RDC, including possible etiological factors; the prevalence of the disease; explaining and showing visually the standard range of the TMJ as well as the alteration found; and, instructing the patient on new habits which could improve the symptomology. Some of these new habits were: maintaining, whenever possible, the relaxed postural position of the mandible (teeth separated, lips lightly touching, tongue touching the anterior part of the hard palate, not pushing against the teeth); positioning the pillow supporting the head and neck during sleep; avoiding placing objects on the chin and/or biting objects; avoiding foods of thick consistency; limiting the maximum range of the oral opening, especially when yawning and laughing; performing bilateral chewing, simultaneously, in order not to overtax the muscles and/or joint individually; placing warm compresses, alternating every 20 minutes. Subsequently, the patient would be molded for the construction of the plane flat OS. At the end of this session, the patient received a new VAS to be filled out during the week in which that patient would incorporate these habits, newly-acquired from the counseling.
At the third appointment, 7 days after counseling, the patient returned to deliver the VAS and for installation of the OS (Figure 2), adjustment of the occlusal contacts (Figure 3), configuration with simultaneous bilateral contacts during closing (Figure 4) and lateral disclusion by canine guide (Figure 5), and protrusion performed by the anterior teeth and disclusion on the posterior teeth. Instructions for the use (24 hours, in the first week) and hygiene of the device were provided, besides receiving another VAS. At the fourth appointment, one week after installation of the OS, the patient delivered the VAS and the occlusal contacts were reassessed. For the other appointments, the follow up intervals became broader, at 15, 30 and 60 days from this fourth session.
Configuration of simultaneous bilateral oclusal contacts during the mandibular closure and canine disclusion (in red).
Having all the VAS, measurements of pain intensities were made. These data were analyzed using the 2-way Analysis of Variance and the Tukey parametric test (p<0.05).
RESULT
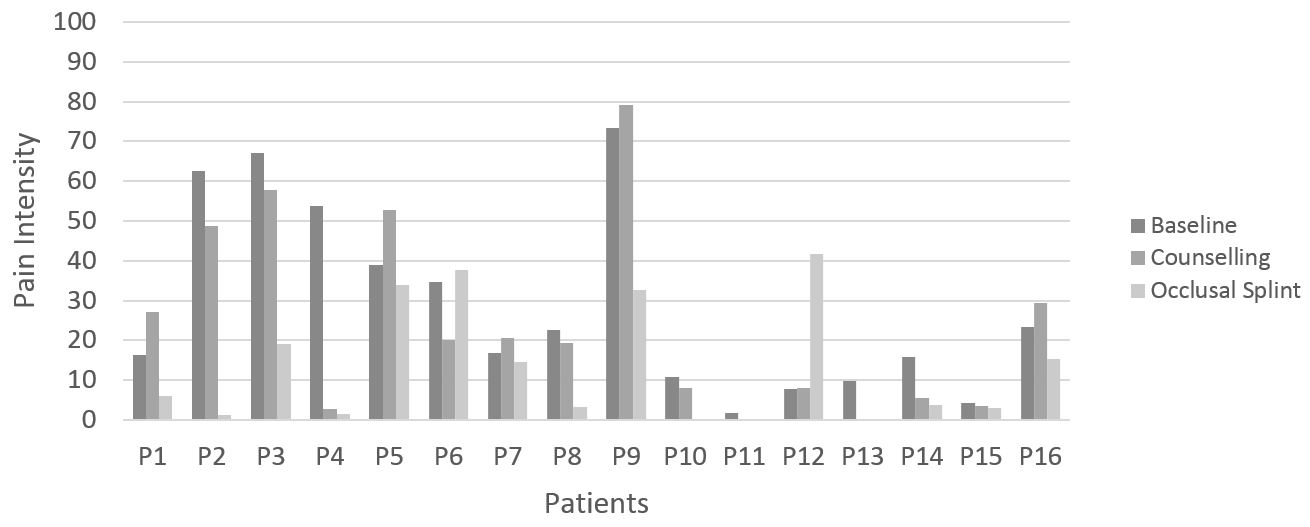
The values obtained from the VAS represent, quantitatively, the intensity of pain that the patients recorded during all stages of the study: after the initial exam, after counseling and subsequent installation of the OS. Thus, the values obtained were divided by 7 days, which represents the interval between appointments. All data are in Table 1.
Measurement, in mm, of pain intensity gotten by VAS after initial exam, after counseling and after OS installation periods
Analyzing the means of the intensity of pain of all patients in the 3 evaluation periods, initial, post-counseling and post-installation of the OS, a reduction in symptomology was found. A reduction in pain intensity was noted in 10 patients after counseling and in 14 patients after the installation of the OS, when compared to the initial data (Figure 6).
When the mean values of the baseline were compared with those of the post-counseling, there was no statistically significant difference, even noting a reduction in pain intensity values. When comparing the means of the patients between the post-counseling periods and the post-installation of the OS, no statistically significant difference was found. However, a reduction in the intensity of the pain reported by the patients was noted. The comparison of the data taken in the moments following the initial exam and after the final analysis showed a statistically significant difference in the reduction of pain symptomology (Figure 7).
DISCUSSION
The objective of the present study was to evaluate the symptomology of patients treated using the association between counseling and an occlusal splint. The patients treated show the trend for TMD among females (100%) with a mean age of 36.6 years, in the age range characteristic for the prevalence of TMD as shown in the literature77 Macfarlane TV, Blinkhorn AS, Davies RM, Kincey J, Worthington HV. Oro-facial pain in the community: prevalence and associated impact. Community Dent Oral Epidemiol. 2002 Feb;30(1):52-60. http://dx.doi.org/10.1034/j.1600-0528.2002.300108.x. PMid:11918576.
http://dx.doi.org/10.1034/j.1600-0528.20...
,88 Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain. 1999;13(4):232-7. PMid:10823035..
All patients who participated in the present study presented with a diagnosis of myofascial pain (Group Ia or Ib – RDC/TMD). Myofascial pain is a condition of regional myogenic pain characterized by hypersensitive localized areas of firm muscle tissues, known as trigger points that represent the most common clinical characteristic of myofascial pain99 Okeson JP. Tratamento das desordens temporomandibulares e oclusão. 6th ed. Rio de Janeiro: Elsevier; 2008.. Palpation produces pain, but the most common symptom is usually associated with excitatory effects of the trigger points, which induce referred pain99 Okeson JP. Tratamento das desordens temporomandibulares e oclusão. 6th ed. Rio de Janeiro: Elsevier; 2008..
The treatment for myofascial pain involves several modalities ranging from conservative to more invasive measures1010 Freitas RF, Ferreira MÂ, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: a systematic review. J Oral Rehabil. 2013 Nov;40(11):864-74. http://dx.doi.org/10.1111/joor.12098. PMid:24102692.
http://dx.doi.org/10.1111/joor.12098...
. Among the options, the occlusal splint, either in isolation or in combination with other modes of treatment, is the most common form of pain control in patients with TMD66 Truelove E, Huggins KH, Mancl L, Dworkin SF. The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: a randomized controlled trial. J Am Dent Assoc. 2006 Aug;137(8):1099-107, quiz 1169. http://dx.doi.org/10.14219/jada.archive.2006.0348. PMid:16873325.
http://dx.doi.org/10.14219/jada.archive....
,1111 Fricton J. Current evidence providing clarity in management of temporomandibular disorders: summary of a systematic review of randomized clinical trials for intra-oral appliances and occlusal therapies. J Evid Based Dent Pract. 2006 Mar;6(1):48-52. http://dx.doi.org/10.1016/j.jebdp.2005.12.020. PMid:17138397.
http://dx.doi.org/10.1016/j.jebdp.2005.1...
12 Wassell RW, Adams N, Kelly PJ. The treatment of temporomandibular disorders with stabilizing splints in general dental practice: one-year follow-up. J Am Dent Assoc. 2006 Aug;137(8):1089-98, quiz 1168-9. http://dx.doi.org/10.14219/jada.archive.2006.0347. PMid:16873324.
http://dx.doi.org/10.14219/jada.archive....
13 Ekberg E, Nilner M. Treatment outcome of appliance therapy in temporomandibular disorder patients with myofascial pain after 6 and 12 months. Acta Odontol Scand. 2004 Dec;62(6):343-9. http://dx.doi.org/10.1080/00016350410010063. PMid:15848979.
http://dx.doi.org/10.1080/00016350410010...
14 Wassell RW, Adams N, Kelly PJ. Treatment of temporomandibular disorders by stabilising splints in general dental practice: results after initial treatment. Br Dent J. 2004 Jul;197(1):35-41, discussion 31, quiz 50-1. http://dx.doi.org/10.1038/sj.bdj.4811420. PMid:15243608.
http://dx.doi.org/10.1038/sj.bdj.4811420...
15 Ekberg E, Vallon D, Nilner M. The efficacy of appliance in patients with temporomandibular disorders of mainly myogenous origin. A randomized, controlled, short-term trial. J Orofac Pain. 2003;17(2):133-9. PMid:12836501.
16 Ekberg EC, Vallon D, Nilner M. Occlusal appliance therapy in patients with temporomandibular disorders a double-blind controlled study in a short-term perspective. Acta Odontol Scand. 1998 Apr;56(2):122-8. http://dx.doi.org/10.1080/00016359850136102. PMid:9669465.
http://dx.doi.org/10.1080/00016359850136...
-1717 Rubinoff MS, Gross A, McCall WP Jr. Conventional and nonoccluding splint therapy compared for patient with myofascial pain dysfunction syndrome. Gen Dent. 1987 Nov-Dec;35(6):502-6. PMid:3481734.. A systematic review by Freitas et al.1010 Freitas RF, Ferreira MÂ, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: a systematic review. J Oral Rehabil. 2013 Nov;40(11):864-74. http://dx.doi.org/10.1111/joor.12098. PMid:24102692.
http://dx.doi.org/10.1111/joor.12098...
revealed the effectiveness of counseling and self-control therapies for the treatment of myofascial TMD, compared with the use of the occlusal splint. They found similar results between the therapies for spontaneous pain, muscular rigidity upon palpation and maximum opening with or without pain.
The present study revealed an improvement in the symptomology following the installation of the splint, when compared with the initial data and after counseling. The action mechanisms of the OS are not completely clear, and several hypotheses are proposed to explain its effectiveness1818 Scopel V, Alves da Costa GS, Urias D. An electromyographic study of masseter and anterior temporalis muscles in extra-articular myogenous TMJ pain patients compared to an asymptomatic and normal population. Cranio. 2005 Jul;23(3):194-203. http://dx.doi.org/10.1179/crn.2005.028. PMid:16128354.
http://dx.doi.org/10.1179/crn.2005.028...
19 Dubé C, Rompré PH, Manzini C, Guitard F, de Grandmont P, Lavigne GJ. Quantitative polygraphic controlled study on efficacy and safety of oral splint devices in tooth-grinding subjects. J Dent Res. 2004 May;83(5):398-403. http://dx.doi.org/10.1177/154405910408300509. PMid:15111632.
http://dx.doi.org/10.1177/15440591040830...
20 Turp JC, Komine F, Hugger A. Efficacy of stabilization splints for the management of patients with masticatory muscle pain: a qualitative systematic review. Clin Oral Investig. 2004 Dec;8(4):179-95. http://dx.doi.org/10.1007/s00784-004-0265-4. PMid:15179561.
http://dx.doi.org/10.1007/s00784-004-026...
21 Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances: evidence of their efficacy. J Am Dent Assoc. 2001 Jun;132(6):770-7. http://dx.doi.org/10.14219/jada.archive.2001.0274. PMid:11433856.
http://dx.doi.org/10.14219/jada.archive....
22 Yap AU. Effects of stabilization appliance on nocturnal parafunctional activities in patients with and without signs of temporomandibular disorders. J Oral Rehabil. 1998 Jan;25(1):64-8. http://dx.doi.org/10.1046/j.1365-2842.1998.00194.x. PMid:9502129.
http://dx.doi.org/10.1046/j.1365-2842.19...
-2323 Dao TTT, Lavigne GJ, Charbonneau A, Feine JS, Lund JP. The efficacy of oral splints in the treatment of myofascial pain of the jaw muscles: a controlled clinical trial. Pain. 1994 Jan;56(1):85-94. http://dx.doi.org/10.1016/0304-3959(94)90153-8. PMid:8159444.
http://dx.doi.org/10.1016/0304-3959(94)9...
. A few assumptions may be cited: alteration of the positions of the condyles and/or the articulator disks in the TMJ; reduction of electromyographic activity of the masticatory muscles; modifications in parafunctional activities; changes in the occlusal condition of the patients and in the vertical dimension; change in the peripheral impulses (motor or afferent) to the central nervous system; greater awareness of the patient; cognitive placebo effect99 Okeson JP. Tratamento das desordens temporomandibulares e oclusão. 6th ed. Rio de Janeiro: Elsevier; 2008.,1919 Dubé C, Rompré PH, Manzini C, Guitard F, de Grandmont P, Lavigne GJ. Quantitative polygraphic controlled study on efficacy and safety of oral splint devices in tooth-grinding subjects. J Dent Res. 2004 May;83(5):398-403. http://dx.doi.org/10.1177/154405910408300509. PMid:15111632.
http://dx.doi.org/10.1177/15440591040830...
,2121 Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances: evidence of their efficacy. J Am Dent Assoc. 2001 Jun;132(6):770-7. http://dx.doi.org/10.14219/jada.archive.2001.0274. PMid:11433856.
http://dx.doi.org/10.14219/jada.archive....
,2424 Ekberg E, Nilner M. A 6-and 12 month follow-up of appliance therapy in TMD patients: a follow-up of a controlled trial. Int J Prosthodont. 2002 Nov-Dec;15(6):564-70. PMid:12475163.
25 Widmalm SE. Use and abuse of bite splints. Compend Contin Educ Dent. 1999 Mar;20(3):249-54, 256, 258-9, quiz 260. PMid:11692335.-2626 Okeson JP. The effects of hard and soft occlusal splints on nocturnal bruxism. J Am Dent Assoc. 1987 Jun;114(6):788-91. http://dx.doi.org/10.14219/jada.archive.1987.0165. PMid:3475357.
http://dx.doi.org/10.14219/jada.archive....
.
The plane flat rigid plate can be used to control signs and symptoms in inflammatory muscle and joint disorders, also for protection against excessive tooth wear caused by bruxism during sleep and/or teeth clenching2727 Magdaleno F, Ginestal E. Side effects of stabilization occlusal splints: a report of three cases and literature review. Cranio. 2010 Apr;28(2):128-35. http://dx.doi.org/10.1179/crn.2010.018. PMid:20491235.
http://dx.doi.org/10.1179/crn.2010.018...
. Widmalm2525 Widmalm SE. Use and abuse of bite splints. Compend Contin Educ Dent. 1999 Mar;20(3):249-54, 256, 258-9, quiz 260. PMid:11692335. adds that the OS is effective for testing the effects that changes in occlusion could have on the function of the TMJ and the masticatory muscles prior to restorative treatment, when finding the influence of the occlusion on the disorder.
It is estimated that the effectiveness of the OS in reducing TMD symptoms is between 70 and 90%1212 Wassell RW, Adams N, Kelly PJ. The treatment of temporomandibular disorders with stabilizing splints in general dental practice: one-year follow-up. J Am Dent Assoc. 2006 Aug;137(8):1089-98, quiz 1168-9. http://dx.doi.org/10.14219/jada.archive.2006.0347. PMid:16873324.
http://dx.doi.org/10.14219/jada.archive....
, when used in association with other methods of treatment. Based on the data recorded by the patients of this case report, a reduction was found in the mean pain intensity in patients among the moments evaluated. This reduction was significant only when the post-installation data for the OS were compared to the initial and post-counseling data. The objective of any treatment modality for myofascial pain is to relieve or eliminate the symptom as well as to reestablish muscular function55 Alencar F Jr, Becker A. Evaluation of different occlusal splints and counselling in the management of myofascial pain dysfunction. J Oral Rehabil. 2009 Feb;36(2):79-85. http://dx.doi.org/10.1111/j.1365-2842.2008.01913.x. PMid:18976268.
http://dx.doi.org/10.1111/j.1365-2842.20...
. The myorelaxant occlusal splints may improve the pain and the amplitude of the mandibular movements significantly. Thus, it is considered an effective treatment for patients with myofascial pain (Subgroup I) and Dislocated Disks (Subgroup II)2828 Botelho LC, Messora MR, Pereira CV, Pereira SM, Marques LS, Pereira LJ. Estudo longitudinal dos sinais e sintomas de disfunção temporomandibular frente a tratamento conservador com placa estabilizadora em clínica de graduação. Arq Odontol. 2012 Abr-Jun;48(2):76-81. http://dx.doi.org/10.7308/aodontol/2012.48.2.03.
http://dx.doi.org/10.7308/aodontol/2012....
.
Alencar, Becker55 Alencar F Jr, Becker A. Evaluation of different occlusal splints and counselling in the management of myofascial pain dysfunction. J Oral Rehabil. 2009 Feb;36(2):79-85. http://dx.doi.org/10.1111/j.1365-2842.2008.01913.x. PMid:18976268.
http://dx.doi.org/10.1111/j.1365-2842.20...
claimed that the treatment of patients with myofascial pain should involve low-cost, conservative therapies (counseling and self-care). They also claimed that the type of format or material of the OS did not affect the results between the groups using the rigid, soft and uncovered interocclusal splints, when only the reduction of pain intensity after treatment was analyzed.
According to the data from the present study, it was found that some patients had an increase in the intensity of the pain, as seen in patients numbers 1, 5, 7, 9 and 16 after the installation of the OS. It is currently known that biomedical factors and psychosocial impacts are involved in the development of TMD2929 Suvinen TI, Reade PC, Kemppainen P, Könönen M, Dworkin SF. Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005 Dec;9(6):613-33. http://dx.doi.org/10.1016/j.ejpain.2005.01.012. PMid:15978854.
http://dx.doi.org/10.1016/j.ejpain.2005....
. This may explain the increase in pain among these patients, and highlights the need for a biopsychosocial approach that takes into account the multifactorial nature of this disease in addition to an interdisciplinary treatment involving physiological, psychological and social aspects which may trigger or perpetuate the chronic pain of TMD3030 Sherman JJ, Turk DC. Nonpharmacologic approaches to the management of myofascial temporomandibular disorders. Curr Pain Headache Rep. 2001 Oct;5(5):421-31. http://dx.doi.org/10.1007/s11916-001-0053-7. PMid:11560807.
http://dx.doi.org/10.1007/s11916-001-005...
. Thus, the treatment for TMD is characterized as reversible and conservative, and involves self-care strategies and behavioral therapies3131 Dionne RA. Pharmacologic treatments for temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997 Jan;83(1):134-42. http://dx.doi.org/10.1016/S1079-2104(97)90104-9. PMid:9007937.
http://dx.doi.org/10.1016/S1079-2104(97)...
,3232 Feine JS, Widmer CG, Lund JP. Physical therapy: a critique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997 Jan;83(1):123-7. http://dx.doi.org/10.1016/S1079-2104(97)90102-5. PMid:9007935.
http://dx.doi.org/10.1016/S1079-2104(97)...
.
The counseling includes extensive education about the disease and guarantees its benign progress associated with the use of heat or cold therapies, mandible exercises and guidance on reducing parafunctional mandibular activities, progressive muscular relaxation, diaphragmatic breathing training and improved sleep and posture44 Michelotti A, Iodice G, Vollaro S, Steenks MH, Farella M. Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles. J Am Dent Assoc. 2012 Jan;143(1):47-53. http://dx.doi.org/10.14219/jada.archive.2012.0018. PMid:22207667.
http://dx.doi.org/10.14219/jada.archive....
5 Alencar F Jr, Becker A. Evaluation of different occlusal splints and counselling in the management of myofascial pain dysfunction. J Oral Rehabil. 2009 Feb;36(2):79-85. http://dx.doi.org/10.1111/j.1365-2842.2008.01913.x. PMid:18976268.
http://dx.doi.org/10.1111/j.1365-2842.20...
-66 Truelove E, Huggins KH, Mancl L, Dworkin SF. The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: a randomized controlled trial. J Am Dent Assoc. 2006 Aug;137(8):1099-107, quiz 1169. http://dx.doi.org/10.14219/jada.archive.2006.0348. PMid:16873325.
http://dx.doi.org/10.14219/jada.archive....
,3333 Michelotti A, Steenks MH, Farella M, Parisini F, Cimino R, Martina R. The additional value of a home physical therapy regimen versus patient education only for the treatment of myofascial pain of the jaw muscles: short-term results of a randomized clinical trial. J Orofac Pain. 2004;18(2):114-25. PMid:15250431.
34 Carlson CR, Bertrand PM, Ehrlich AD, Maxwell AW, Burton RG. Physical self-regulation training for the management of temporomandibular disorders. J Orofac Pain. 2001;15(1):47-55. PMid:11889647.-3535 Wright EF, Domenech MA, Fischer JR Jr. Usefulness of posture training for patients with temporomandibular disorders. J Am Dent Assoc. 2000 Feb;131(2):202-10. http://dx.doi.org/10.14219/jada.archive.2000.0148. PMid:10680388.
http://dx.doi.org/10.14219/jada.archive....
. This approach does not require profound knowledge of psychology and treatment strategies, such as cognitive-behavioral treatment and psychotherapies1010 Freitas RF, Ferreira MÂ, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: a systematic review. J Oral Rehabil. 2013 Nov;40(11):864-74. http://dx.doi.org/10.1111/joor.12098. PMid:24102692.
http://dx.doi.org/10.1111/joor.12098...
. So this therapy may be applied to the treatment of TMD pain by any professional with experience in the prevention and elimination of possible etiological factors responsible of triggering and perpetuating the signs and symptoms of TMD health1010 Freitas RF, Ferreira MÂ, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: a systematic review. J Oral Rehabil. 2013 Nov;40(11):864-74. http://dx.doi.org/10.1111/joor.12098. PMid:24102692.
http://dx.doi.org/10.1111/joor.12098...
.
Regarding the atteendance of patients to other appointments, after the first follow up appointment of the OS, a considerable reduction was noticed. This suggests that there was a reduction in pain, and confirms that this symptom is primarily responsible for seeking treatment. Additionally, the acquisition of knowledge about the disease and new habits may promote greater longevity in treatment efficacy.
CONCLUSION
According to the data obtained in the present study, the association between counseling and the OS can be found to be an excellent option for the treatment of patients with myofascial pain. In addition to being conservative, non-invasive and low-cost, this therapeutic modality suggests greater longevity in pain reduction because the patient acquires new habits or behaviors which avoid muscular and joint overtaxing.
REFERENCES
-
1Sipilä K, Suominen AL, Alanen P, Heliövaara M, Tiittanen P, Könönen M. Association of clinical findings of temporomandibular disorders (TMD) with self-reported musculoskeletal pains. Eur J Pain. 2011 Nov;15(10):1061-7. http://dx.doi.org/10.1016/j.ejpain.2011.05.001 PMid:21664847.
» http://dx.doi.org/10.1016/j.ejpain.2011.05.001 -
2Nelson SJ. Principles of stabilization bite splint therapy. Dent Clin North Am. 1995 Apr;39(2):403-21. PMid:7781834.
-
3Boero RP. The physiology of splint therapy: a literature review. Angle Orthod. 1989;59(3):165-80. PMid:2672904.
-
4Michelotti A, Iodice G, Vollaro S, Steenks MH, Farella M. Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles. J Am Dent Assoc. 2012 Jan;143(1):47-53. http://dx.doi.org/10.14219/jada.archive.2012.0018 PMid:22207667.
» http://dx.doi.org/10.14219/jada.archive.2012.0018 -
5Alencar F Jr, Becker A. Evaluation of different occlusal splints and counselling in the management of myofascial pain dysfunction. J Oral Rehabil. 2009 Feb;36(2):79-85. http://dx.doi.org/10.1111/j.1365-2842.2008.01913.x PMid:18976268.
» http://dx.doi.org/10.1111/j.1365-2842.2008.01913.x -
6Truelove E, Huggins KH, Mancl L, Dworkin SF. The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: a randomized controlled trial. J Am Dent Assoc. 2006 Aug;137(8):1099-107, quiz 1169. http://dx.doi.org/10.14219/jada.archive.2006.0348 PMid:16873325.
» http://dx.doi.org/10.14219/jada.archive.2006.0348 -
7Macfarlane TV, Blinkhorn AS, Davies RM, Kincey J, Worthington HV. Oro-facial pain in the community: prevalence and associated impact. Community Dent Oral Epidemiol. 2002 Feb;30(1):52-60. http://dx.doi.org/10.1034/j.1600-0528.2002.300108.x PMid:11918576.
» http://dx.doi.org/10.1034/j.1600-0528.2002.300108.x -
8Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain. 1999;13(4):232-7. PMid:10823035.
-
9Okeson JP. Tratamento das desordens temporomandibulares e oclusão. 6th ed. Rio de Janeiro: Elsevier; 2008.
-
10Freitas RF, Ferreira MÂ, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: a systematic review. J Oral Rehabil. 2013 Nov;40(11):864-74. http://dx.doi.org/10.1111/joor.12098 PMid:24102692.
» http://dx.doi.org/10.1111/joor.12098 -
11Fricton J. Current evidence providing clarity in management of temporomandibular disorders: summary of a systematic review of randomized clinical trials for intra-oral appliances and occlusal therapies. J Evid Based Dent Pract. 2006 Mar;6(1):48-52. http://dx.doi.org/10.1016/j.jebdp.2005.12.020 PMid:17138397.
» http://dx.doi.org/10.1016/j.jebdp.2005.12.020 -
12Wassell RW, Adams N, Kelly PJ. The treatment of temporomandibular disorders with stabilizing splints in general dental practice: one-year follow-up. J Am Dent Assoc. 2006 Aug;137(8):1089-98, quiz 1168-9. http://dx.doi.org/10.14219/jada.archive.2006.0347 PMid:16873324.
» http://dx.doi.org/10.14219/jada.archive.2006.0347 -
13Ekberg E, Nilner M. Treatment outcome of appliance therapy in temporomandibular disorder patients with myofascial pain after 6 and 12 months. Acta Odontol Scand. 2004 Dec;62(6):343-9. http://dx.doi.org/10.1080/00016350410010063 PMid:15848979.
» http://dx.doi.org/10.1080/00016350410010063 -
14Wassell RW, Adams N, Kelly PJ. Treatment of temporomandibular disorders by stabilising splints in general dental practice: results after initial treatment. Br Dent J. 2004 Jul;197(1):35-41, discussion 31, quiz 50-1. http://dx.doi.org/10.1038/sj.bdj.4811420 PMid:15243608.
» http://dx.doi.org/10.1038/sj.bdj.4811420 -
15Ekberg E, Vallon D, Nilner M. The efficacy of appliance in patients with temporomandibular disorders of mainly myogenous origin. A randomized, controlled, short-term trial. J Orofac Pain. 2003;17(2):133-9. PMid:12836501.
-
16Ekberg EC, Vallon D, Nilner M. Occlusal appliance therapy in patients with temporomandibular disorders a double-blind controlled study in a short-term perspective. Acta Odontol Scand. 1998 Apr;56(2):122-8. http://dx.doi.org/10.1080/00016359850136102 PMid:9669465.
» http://dx.doi.org/10.1080/00016359850136102 -
17Rubinoff MS, Gross A, McCall WP Jr. Conventional and nonoccluding splint therapy compared for patient with myofascial pain dysfunction syndrome. Gen Dent. 1987 Nov-Dec;35(6):502-6. PMid:3481734.
-
18Scopel V, Alves da Costa GS, Urias D. An electromyographic study of masseter and anterior temporalis muscles in extra-articular myogenous TMJ pain patients compared to an asymptomatic and normal population. Cranio. 2005 Jul;23(3):194-203. http://dx.doi.org/10.1179/crn.2005.028 PMid:16128354.
» http://dx.doi.org/10.1179/crn.2005.028 -
19Dubé C, Rompré PH, Manzini C, Guitard F, de Grandmont P, Lavigne GJ. Quantitative polygraphic controlled study on efficacy and safety of oral splint devices in tooth-grinding subjects. J Dent Res. 2004 May;83(5):398-403. http://dx.doi.org/10.1177/154405910408300509 PMid:15111632.
» http://dx.doi.org/10.1177/154405910408300509 -
20Turp JC, Komine F, Hugger A. Efficacy of stabilization splints for the management of patients with masticatory muscle pain: a qualitative systematic review. Clin Oral Investig. 2004 Dec;8(4):179-95. http://dx.doi.org/10.1007/s00784-004-0265-4 PMid:15179561.
» http://dx.doi.org/10.1007/s00784-004-0265-4 -
21Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances: evidence of their efficacy. J Am Dent Assoc. 2001 Jun;132(6):770-7. http://dx.doi.org/10.14219/jada.archive.2001.0274 PMid:11433856.
» http://dx.doi.org/10.14219/jada.archive.2001.0274 -
22Yap AU. Effects of stabilization appliance on nocturnal parafunctional activities in patients with and without signs of temporomandibular disorders. J Oral Rehabil. 1998 Jan;25(1):64-8. http://dx.doi.org/10.1046/j.1365-2842.1998.00194.x PMid:9502129.
» http://dx.doi.org/10.1046/j.1365-2842.1998.00194.x -
23Dao TTT, Lavigne GJ, Charbonneau A, Feine JS, Lund JP. The efficacy of oral splints in the treatment of myofascial pain of the jaw muscles: a controlled clinical trial. Pain. 1994 Jan;56(1):85-94. http://dx.doi.org/10.1016/0304-3959(94)90153-8 PMid:8159444.
» http://dx.doi.org/10.1016/0304-3959(94)90153-8 -
24Ekberg E, Nilner M. A 6-and 12 month follow-up of appliance therapy in TMD patients: a follow-up of a controlled trial. Int J Prosthodont. 2002 Nov-Dec;15(6):564-70. PMid:12475163.
-
25Widmalm SE. Use and abuse of bite splints. Compend Contin Educ Dent. 1999 Mar;20(3):249-54, 256, 258-9, quiz 260. PMid:11692335.
-
26Okeson JP. The effects of hard and soft occlusal splints on nocturnal bruxism. J Am Dent Assoc. 1987 Jun;114(6):788-91. http://dx.doi.org/10.14219/jada.archive.1987.0165 PMid:3475357.
» http://dx.doi.org/10.14219/jada.archive.1987.0165 -
27Magdaleno F, Ginestal E. Side effects of stabilization occlusal splints: a report of three cases and literature review. Cranio. 2010 Apr;28(2):128-35. http://dx.doi.org/10.1179/crn.2010.018 PMid:20491235.
» http://dx.doi.org/10.1179/crn.2010.018 -
28Botelho LC, Messora MR, Pereira CV, Pereira SM, Marques LS, Pereira LJ. Estudo longitudinal dos sinais e sintomas de disfunção temporomandibular frente a tratamento conservador com placa estabilizadora em clínica de graduação. Arq Odontol. 2012 Abr-Jun;48(2):76-81. http://dx.doi.org/10.7308/aodontol/2012.48.2.03
» http://dx.doi.org/10.7308/aodontol/2012.48.2.03 -
29Suvinen TI, Reade PC, Kemppainen P, Könönen M, Dworkin SF. Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005 Dec;9(6):613-33. http://dx.doi.org/10.1016/j.ejpain.2005.01.012 PMid:15978854.
» http://dx.doi.org/10.1016/j.ejpain.2005.01.012 -
30Sherman JJ, Turk DC. Nonpharmacologic approaches to the management of myofascial temporomandibular disorders. Curr Pain Headache Rep. 2001 Oct;5(5):421-31. http://dx.doi.org/10.1007/s11916-001-0053-7 PMid:11560807.
» http://dx.doi.org/10.1007/s11916-001-0053-7 -
31Dionne RA. Pharmacologic treatments for temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997 Jan;83(1):134-42. http://dx.doi.org/10.1016/S1079-2104(97)90104-9 PMid:9007937.
» http://dx.doi.org/10.1016/S1079-2104(97)90104-9 -
32Feine JS, Widmer CG, Lund JP. Physical therapy: a critique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997 Jan;83(1):123-7. http://dx.doi.org/10.1016/S1079-2104(97)90102-5 PMid:9007935.
» http://dx.doi.org/10.1016/S1079-2104(97)90102-5 -
33Michelotti A, Steenks MH, Farella M, Parisini F, Cimino R, Martina R. The additional value of a home physical therapy regimen versus patient education only for the treatment of myofascial pain of the jaw muscles: short-term results of a randomized clinical trial. J Orofac Pain. 2004;18(2):114-25. PMid:15250431.
-
34Carlson CR, Bertrand PM, Ehrlich AD, Maxwell AW, Burton RG. Physical self-regulation training for the management of temporomandibular disorders. J Orofac Pain. 2001;15(1):47-55. PMid:11889647.
-
35Wright EF, Domenech MA, Fischer JR Jr. Usefulness of posture training for patients with temporomandibular disorders. J Am Dent Assoc. 2000 Feb;131(2):202-10. http://dx.doi.org/10.14219/jada.archive.2000.0148 PMid:10680388.
» http://dx.doi.org/10.14219/jada.archive.2000.0148
Publication Dates
-
Publication in this collection
04 Aug 2016 -
Date of issue
Jul-Aug 2016
History
-
Received
26 Dec 2015 -
Accepted
09 May 2016