Abstracts
Testicular and penile cancers are genital disorders that affect a small part of population, but are generally aggressive mainly because of the dramatic psychological effect they impose over patients. The purpose of this study was to identify evidence concerning preventing strategies for the referred types of cancer. An integrative literature review was performed on the COCHRANE, PubMed/MEDLINE, LILACS, BDENF and CINAHL databases using the following controlled descriptors: health promotion, risk factors, primary prevention, and urogenital neoplasms; and uncontrolled descriptors: prevention, penile cancer, testicle cancer. The studies were unanimous in concluding that self-examination of testicles is the best way to identify a possible event of testicular cancer. Circumcision, prevention for sexual transmission diseases and adequate hygiene were the most important manners for penile cancer prevention. Nurses should assume the role for general and specific health promotion, considering the major impact it would have for prevention of diseases, especially for the urogenital cancers studied in this review.
Genital neoplasms, male; Risk factors; Primary prevention; Oncologic nursing
Cânceres de testículo e pênis são doenças que acometem pequena parcela da população, mas geralmente são agressivas principalmente pelo impacto psicológico que exercem sobre os pacientes. Este estudo buscou identificar evidências de estratégias preventivas para tais cânceres. Foi realizada revisão integrativa de literatura, nas bases de dados Biblioteca COCHRANE, PubMed/MEDLINE, LILACS, BDENF e CINAHL, utilizando os descritores controlados: promoção da saúde, fatores de risco, prevenção primária e neoplasias urogenitais; e os não controlados: prevenção, câncer de pênis, câncer de testículo. Os estudos foram unânimes ao identificar, para o câncer de testículo, o autoexame do órgão; para o câncer de pênis, evidenciou-se a circuncisão como fator protetor, a prevenção de infecção sexualmente transmissível e a adequada higiene íntima. Os enfermeiros devem assumir a função de promotor da saúde, tendo em vista a importância dessa atitude frente à prevenção de doenças.
Neoplasias dos genitais masculinos; Fatores de risco; Prevenção primária; Enfermagem oncológica
El cáncer de testículo y de pene son enfermedades sufridas por un pequeño segmento de la población, generalmente son agresivas, sobre todo por el impacto psicológico que ejercen sobre los pacientes. Este estudio buscó identificar evidencias de estrategias preventivas para tales cánceres. Se realizó una revisión integradora de literatura en las bases de datos Biblioteca COCHRANE, PubMed/MEDLINE, LILACS, BDENF y CINAHL, utilizando los descriptores controlados: promoción de la salud, factores de riesgo, prevención primaria y neoplasias urogenitales; y los no controlados: prevención, cáncer de pene, cáncer de testículo. Los estudios fueron unánimes al identificar, para el cáncer de testículo, el autoexamen del órgano; para el cáncer de pene se evidenció que la circuncisión es un factor de protección, así como la prevención de la infección sexualmente transmisible y la adecuada higiene íntima. Los enfermeros deben asumir la función de promotor de la salud, teniendo en vistas la importancia de tal actitud en la prevención sanitaria.
Neoplasias de los genitales masculinos; Factores de riesgo; Prevención primaria; Enfermería oncológica
ORIGINAL ARTICLE
Kelly Wanessa de SouzaI; Paula Elaine Diniz dos ReisII; Isabelle Pimentel GomesIII; Emília Campos de CarvalhoIV
IRN. Oncology Nursing Specialist, Centro Universitário Unieuro. Brasília, DF, Brazil. Brazil. kwanessa@gmail.com
IIOncology Nurse. Adjunct Professor, Nursing Department, Faculty of Health Sciences, University of Brasília. Brasília, DF, Brazil. pauladiniz@unb.br
IIIOncology Nurse, Instituto Nacional do Câncer. Master's student in Nursing, Federal University of Paraíba. Nurse, Pediatric Clinic, Hospital Universitário Lauro Wanderley, Federal University of Paraíba. João Pessoa, PB, Brazil. enfisabelle@yahoo.com.br
IVFull Professor, University of São Paulo at Ribeirão Preto College of Nursing. Member of the WHO Collaborating Centre for Nursing Research Development. Ribeirão Preto, SP, Brazil. ecdcava@eerp.usp.br
Correspondence addressed to
ABSTRACT
Testicular and penile cancers are genital disorders that affect a small part of population, but are generally aggressive mainly because of the dramatic psychological effect they impose over patients. The purpose of this study was to identify evidence concerning preventing strategies for the referred types of cancer. An integrative literature review was performed on the COCHRANE, PubMed/MEDLINE, LILACS, BDENF and CINAHL databases using the following controlled descriptors: health promotion, risk factors, primary prevention, and urogenital neoplasms; and uncontrolled descriptors: prevention, penile cancer, testicle cancer. The studies were unanimous in concluding that self-examination of testicles is the best way to identify a possible event of testicular cancer. Circumcision, prevention for sexual transmission diseases and adequate hygiene were the most important manners for penile cancer prevention. Nurses should assume the role for general and specific health promotion, considering the major impact it would have for prevention of diseases, especially for the urogenital cancers studied in this review.
Key words: Genital neoplasms, male. Risk factors. Primary prevention. Oncologic nursing.
RESUMEN
El cáncer de testículo y de pene son enfermedades sufridas por un pequeño segmento de la población, generalmente son agresivas, sobre todo por el impacto psicológico que ejercen sobre los pacientes. Este estudio buscó identificar evidencias de estrategias preventivas para tales cánceres. Se realizó una revisión integradora de literatura en las bases de datos Biblioteca COCHRANE, PubMed/MEDLINE, LILACS, BDENF y CINAHL, utilizando los descriptores controlados: promoción de la salud, factores de riesgo, prevención primaria y neoplasias urogenitales; y los no controlados: prevención, cáncer de pene, cáncer de testículo. Los estudios fueron unánimes al identificar, para el cáncer de testículo, el autoexamen del órgano; para el cáncer de pene se evidenció que la circuncisión es un factor de protección, así como la prevención de la infección sexualmente transmisible y la adecuada higiene íntima. Los enfermeros deben asumir la función de promotor de la salud, teniendo en vistas la importancia de tal actitud en la prevención sanitaria.
Descriptores: Neoplasias de los genitales masculinos. Factores de riesgo. Prevención primaria. Enfermería oncológica.
INTRODUCTION
Penile cancer is one of the most ancient diseases known(1). The mutilating nature of surgical treatment affects patients' physical and psychological aspects. Moreover, clinical therapeutic results show high toxicity and low efficacy, and studies still present low evidence and recommendation levels, so that penile cancer can be considered one of the most dangerous tumor affecting men(2). Its incidence is related to men older than 50 years - although young men can also be affected - especially in case of low socioeconomic and education conditions, bad intimate hygiene and non circumcised individuals. Specifically in Brazil, penile cancer represents 2% of all cancer cases in the male population and is more frequent in the North and Northeast than in the South and Southeast. It should be highlighted that, in the regions with the highest incidence levels, penile cancer exceeds prostate and bladder cancer cases(1).
Testicular cancer, on the other hand, mainly affects men between 15 and 40 years old, and incidence levels show about five cases for every 100 thousand individuals(1,3). In comparison with other cancers in the male population, testicular cancer shows low mortality rates(4). Its higher incidence among young and sexually active men stands out, so that this cancer can be mixed up with or even masked by orchiepididymitis(5); which tends to be sexually transmitted. Nowadays, testicular cancer is considered one of the most curable types, mainly if detected early(1).
Although penile and testicular cancers affect a small part of the population, in general, they are always aggressive and provoke a strong psychological impact in patients(6-7). Hence, research on their causes and risk factors is extremely important to decrease their occurrence, as early diagnosis is fundamental for their control and eradication(1,5). This study aims to identify available evidence in literature on penile and testicular cancer prevention strategies.
METHOD
The following research question guided this integrative literature review(8): What evidence exists about possible prevention strategies for testicular and penile cancer?. Inclusion criteria were: studies on penile and testicular cancer prevention; written in English, Portuguese or Spanish; without restriction as to methodological design, published until 2008. Three authors searched the databases Cochrane, PubMed/MEDLINE, LILACS and CINAHL, crossing the controlled descriptors (DeCS/MeSH): promoção da saúde [health promotion], fatores de risco [risk factors], prevenção primária [primary prevention] and neoplasias urogenitais [urogenital neoplasms]; and non-controlled descriptors: prevenção [prevention], câncer de pênis [penile cancer], câncer de testículo [testicular cancer]. The documents were located through bibliographic commutation, access to online collections and e-mail requests to authors. The papers were ranked according to evidence level(9) and degree of recommendation(10); i.e.: evidence level 1 - Systematic review; 2 - Randomized clinical trial; 3 - Cohort; 4 - Case Control; 5 - Case series; 6 - Expert opinion; 7 - Preclinical study. One author(8) considers that the highest validity and reliability levels are numbers 1 and 2, and the lowest numbers 6 and 7. Regarding the degree of recommendation(9); this is classified as: A) result that permits recommending the intervention; B) result that is inconclusive or insufficient to confirm the hypothesis; C) result that contra-indicates the intervention.
RESULTS
Eighteen articles were identified, 4 of which were excluded, 3 due to the language and 1 because it addressed cancer treatment. Fourteen papers were selected, 11 of which published in English. In Brazil, 3 papers discussed penile cancer prevention. With regard to the year of publication, frequencies are higher in the last decade (Chart 1). As for the methodological design, one (7.2%) study was a systematic review and meta-analysis, six (42.8%) were cohort studies, one (7.2%) was a case series, two (14.3%) were expert opinions and four (28.5%) were literature reviews.
Regarding evidence for prevention, the studies unanimously identified self-exam of the organ as a prevention strategy for testicular cancer(12-19). Only two studies(12,18) did not present sufficient results to confirm the hypothesis, while all others(13-15,19) showed a high degree of recommendation. Orchiopexy was presented as an option for high-risk children(20-21). For penile cancer, circumcision was evidenced as a protective factor, as well as self-exam, prevention of sexually transmissible infection and adequate intimate hygiene as prevention strategies(11,19,22-24).
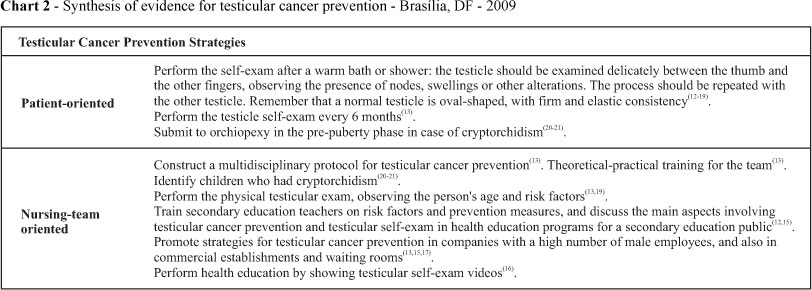
Testicular cancer prevention
The relevance of inserting health education programs to prevent testicular cancer was highlighted, and the importance of nurses' role in this activity was underlined, as survival rates for this type of cancer are directly related with early detection(13). Health education should start with male adolescents, emphasizing the importance of the testicular self-exam(12); which should be performed every six months(13). Some of these authors(12) defend putting in practice this intervention strategy as a part of high school educative activities, covering the age range in which the incidence of this cancer type starts, i.e. 15 years.
In a study(14) that analyzed knowledge on testicular cancer and the accomplishment of the self-exam among 213 adolescents with a mean age of 15.4 years, it was verified that 73% of the adolescents had already heard about the disease, although the self-exam was little practiced among them (10.3% mentioned doing it). The authors recommend making effort to disseminate information on testicular cancer, as well as on the relevance of early diagnosis.
Another study(15) developed in Sweden, involving 727 male adolescents with a mean age of 17 years, aimed to assess knowledge and attitudes regarding testicular cancer and the prevalence of the testicular self-exam. The results showed that most students had never heard of testicular cancer or testicular self-exam, had limited knowledge on common symptoms and hardly ever performed the testicle self-exam. The authors recommend the development of preventive education strategies, suggesting that the subject be included in schools and during military draft definitions.
Visual testicle self-exam testing has been considered an alternative and effective strategy(16). Therefore, the authors developed a video on prostate and testicle cancer prevention, presented to a deaf group of different ages. After the presentation of the video, the participants showed significant understanding about the theme, to the extent that, two months after the presentation, they were reassessed and a high level of knowledge retention was verified.
Testicle cancer prevention should also be part of occupational intervention plans. Strategies should range from nursing consultations to lectures, educative videos and even hanging up posters showing the testicle self-exam step by step in company bathrooms, so that workers are encouraged to perform it(17).
In a convenience sample of 191 patients, 64 men who worked for an American industry indicated that they did not perform the testicle self-exam. Lack of information, region of origin (African, American and Hispanic), low esteem and family conflicts were attributed as the main causes(18).
Besides the self-exam, the American Cancer Society (ACS) recommends a three-annual testicle exam for men over 20 years of age, and every year for men over 40(19). Orchiopexy in the pre-puberty phase can decrease the risk of testicular cancer(20-21). Hence, this surgical intervention is recommended in boys between 10 and 11 years old who had cryptorchidism (failure of the testis to descend during fetal development)(20).
Chart 2 shows the synthesis of testicular cancer prevention strategies presented in the selected articles.
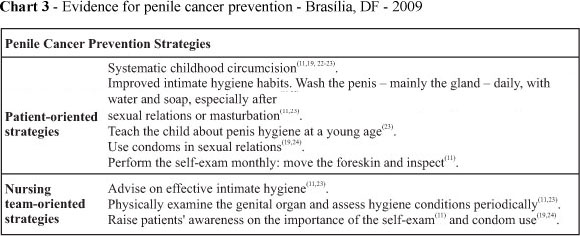
Penile cancer prevention
The direct relation between penile cancer incidence and childhood circumcision was evidenced in a study(11) that monitored 811 patients for 31 years. Circumcision revealed to be a protective factor and practice that should be stimulated in risk populations. Besides, adequate hygiene is considered an additional factor for penile cancer prevention. The same study affirms that the association between circumcision(11,22) and penis hygiene could drastically reduce incidence levels of the disease(11).
In an epidemiological study carried out in the State of Pará, 346 patients from interior regions were analyzed. The age range of their disease (65%) varied between 40 and 69 years. Common factors included lack of circumcision and precarious hygiene habits. Thus, the authors(23) suggest that childhood circumcision and improved genital hygiene habits can be effective means to prevent the disease. It is highlighted, however, that the protective effect is circumcision is acknowledged for localized and invasive cancer, but not for in situ carcinoma(19).
Despite the unknown etiology, studies related HPV and penile cancer(19,24); with findings of DNA-HPV associated with the disease ranging between 15% and 46.3% and a higher presence of subtype 16(24). Other risk factors are also associated with this disease, such as phimosis, chronic inflammatory conditions, photochemotherapy with ultraviolet A rays and smoking.
Chart 3 shows the synthesis of penile cancer prevention strategies presented in the selected articles.
DISCUSSION
It is perceived that testicular and penile cancer prevention strategies are related with socioeconomic issues, mainly education, which can have a determinant influence on countless diseases that affect the population's health.
Knowledge on risk factors(1,14,16-17,20-21); including: age range with highest incidence levels, cryptorchidism, previous testicular tumor, previous family history of testicular cancer in first degree relatives (father or brother), white ethnic origin and genetic alterations, is relevant for the development of programs directed at this population group(25).
The testicular self-exam is considered the most influential and efficient testicular cancer prevention strategy. Its accomplishment should start to be disseminated by hanging up posters in strategic places(17); such as public transportation, public bathrooms, waiting rooms, and also by using educative videos(15); electronic media and health education for adolescents(13).
Likewise, it is important to highlight the fundamental role of the mother or person responsible for the child in childhood education, in the prevention of testicular and penile cancer, through the establishment of hygiene habits and genital intimate care since a young age. Therefore, it is relevant for pediatrics professionals and educators to heed the development of teaching strategies with a view to determining prevention evidence with long-lasting effects.
In this sense, it is considered relevant, at least from adolescence onwards, to encourage young boys to do the self-exam, including the orientation to mainly observe: presence of node, induration or swelling, which can be accompanied by pain or not. Other alterations should also be observed, such as: increased testicle volume, which can cause feelings of heaviness; asymmetry; local skin alteration(17); which can represent local tumor growth.
Penile cancer is not very frequent in developed countries, corresponding to no more than 0.4% of cancers affecting men. Few years ago, special attention started to be paid to the detection of potentially infectious lesions due to HPV in the male population(26). Especially in regions with higher penile cancer incidence levels, like in the North and Northeast of Brazil, and considering that HPV is the sexually transmitted viral infection that most affects the sexually active population, studies aimed at verifying the relation between penile cancer and the presence of HPV would be highly relevant.
Nurse researchers from the State of Ceará, Brazil have developed an Amplified Genital Photo Mapping technique, a screening and detection exam for clinical and sub-clinical lesions caused by the Human Papillomavirus (HPV) in male genitals. Its use is proposed as a complement to traditional exams(26).
The direct relation between penile cancer and maintaining adequate hygiene standards, as well as the greater or lesser practice of circumcision and the age it is performed, support the idea that the disease can be avoided and that systematic childhood circumcision, as various authors recommend(1,11,22-23); could determine a drastic reduction in the incidence levels of this cancer type.
Finally, educative action to prevent these types of cancers, which are part of basic health actions, should be considered a professional commitment to the population's quality of life and a care quality commitment, emphasizing patients' autonomy in self-care(27). Education should not only be considered an extra activity at health services, but an action that redirects professional practices at health units as a whole.
CONCLUSION
Despite few publications on the theme and the fact that the studies lack the methodological rigor of a trial, most research produced evidence that can be recommended. Thus, the need for further research is highlighted, testing effective testicular and penile cancer prevention forms, performed by nurses active in daily clinical practice with people who are victims of this disease or not, so that more effective prevention strategies are evidenced.
In addition, measures should be developed to encourage the male population to seek information from health services. In care practice, it is perceived that less men than women go to health centers. Public clarification campaigns for the male public need to be elaborated. Due to the lack of information, women assume the sole responsibility for sexual health prevention in the couple. This fact impairs early cancer diagnosis in men for different reasons. In this sense, instructing women on preventive actions for penile and testicular cancer is also considered relevant, as women play a fundamental role in male health care.
Moreover, the HPV vaccine has already been consolidated as a primary prevention measure for uterine colon cancer in women who have not been contaminated yet. The researchers hope that, in the future, significant evidence of vaccination efficacy with protective effects for penile cancer will exist.
REFERENCES
-
1Brasil. Ministério da Saúde. Instituto Nacional de Câncer (INCA). Tipos de câncer: pênis [Internet]. [citado 2008 jun.15]. Disponível em: http://www2.inca.gov.br/wps/wcm/connect/tiposdecancer/site/home/penis
- 2. Protzel C, Klebingat HJ, Hakenberg OW. [Treatment of advanced penile cancer. Do we need new methods for chemotherapy?]. Urologe A. 2008;47(9):1229-32. German
- 3. McCullagh J, Lewis G. Testicular cancer: epidemiology, assessment and management. Nurs Standart. 2005;19(25):45-53.
- 4. World Health Organization (WHO). Cancer mondial [Internet]. Lyon: International Agency for Research on Cancer; 2008 [cited 2010 Apr 10]. Available from: http://www-dep.iarc.fr/WHO_frame.htm
- 5. Marra MO, Silva AL, Toledo RR. Síndrome de Fournier e câncer de testículo: apresentação de caso. Rev Med M Gerais. 2008;18(4):287-9.
- 6. Bullen K, Matthews S, Edwards S, Marke V. Exploring men's experiences of penile cancer surgery to improve rehabilitation. Nurs Times. 2009;105(12):20-4.
- 7. Fleer J, Sleijfer D, Hoekstra H, Tuinman M, Klip E, Hoekstra-Weebers J. Objective and subjective predictors of cancer-related stress symptoms in testicular cancer survivors. Patient Educ Couns. 2006;64(1/3):142-50.
- 8. Mendes KDS, Silveira RCCP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto Contexto Enferm. 2008; 17(4):758-64.
- 9. Atallah NA, Trevisani VFM, Valente O. Princípios para tomadas de decisões terapêuticas com base em evidências científicas. In: Prado FC, Ramos J, Valle JR. Atualização terapêutica. 21Ş ed. Porto Alegre: Artes Médicas; 2003. p. 1704-6.
- 10. Phillips B, Ball C, Sackett D, Badenoch D, Strauss S, Haynes B, et al. Levels of evidence and grades of recommendation [Internet]. Oxford: Centre for Evidence-Based Medicine; 2010 [cited 2008 May 10]. Available from: http://www.cebm.net/?o=1025
- 11. Barbosa Júnior AA, Athanázio PRF, Oliveira B. Câncer do pênis: estudo da sua patologia geográfica no Estado da Bahia, Brasil. Rev Saúde Pública [Internet]. 1984 [citado 2008 maio 10];18(6):429-35. Disponível em: http://www.scielo.br/pdf/rsp/v18n6/02.pdf
- 12. Wohl RE, Kane WM. Teacher's beliefs concerning teaching about testicular cancer and testicular self-examination. J School Health. 1997;67(3):106-11.
- 13. Peate I. Testicular cancer: the importance of effective health education. Br J Nurs. 1997; 6(6):311-6.
- 14. Ward KD, Vander Weg MW, Read MC, Sell MA, Beech BM. Testicular cancer awareness and self-examination among adolescent males in a community-based youth organization. Prev Med. 2005;41(2):386-98.
- 15. Rudberg L, Nilsson S, Wikblad K, Carlsson M. Testicular cancer and testicular self-examination: knowledge and attitudes of adolescent swedish men. Cancer Nurs. 2005;28(4):256-62.
- 16. Folkins A, Sadler GR, Ko C, Branz P, Marsh S, Bovee M. Improving the Deaf community's acess to prostate and testicular cancer information: a survey study. BMC Public Health. 2005;5(1):63-72.
- 17. McCullagh J, Lewis G, Warlow C. Promoting awareness and practice of testicular self-examination. Nurs Stand. 2005;19(51):41-9.
- 18. Wynd CA. Testicular self-examination in young adult men. J Nurs Scholarsh. 2002;34(3):251-5.
- 19. Stotts R C. Cancers of the prostate, penis, and testicles: epidemiology, prevention, and treatment. Nurs Clin North Am. 2004;39(2):327-40.
- 20. Walsh TJ, Dall´Era MA, Croughan MS, Carrol PR, Turek PJ. Prepubertal orchiopexy for cryptorchidism may be associated with lower risk of testicular cancer. J Urol. 2007;178(4 Pt 1):1440-6.
- 21. Wood HM. Orchiopexy may prevent testis cancer in boys with criptorchidism [editorial comment]. J Urol. 2007;178(4 Pt 1):1446.
- 22. Schoen EJ. Penile cancer in elderly circuncised man. J Fam Pract. 1997;45(5):442-3.
- 23. Fonseca AG, Nascimento SS, Alencar RV, Cordeito HP. Câncer de pênis: estudo epidemiológico no estado do Pará. Rev Para Med. 2000;14(1):11-6.
- 24. Carvalho NS, Kannemberg AP, Munareto C, Yoshioka D, Absy MCV, Ferreira MA, et al. Associação entre HPV e câncer peniano: revisão de literatura. J Bras Doenças Sex Transm. 2007;19(2):92-5.
- 25. Tonani M, Carvalho EC. Risco de câncer e comportamentos preventivos: a persuasão como estratégia de intervenção. Rev Lat Am Enferm. 2008;16(5):864-70.
- 26. Franco ES, Franco RGFM, Hypóolito SB, Bezerra SJS, Pagliuca LMF. Fotomapeamento genital ampliado: descrição da técnica. Rev Enferm UERJ. 2005;13(3):299-305.
- 27. Barros DG, Chiesa AM. Autonomia e necessidades de saúde na sistematização da assistência de enfermagem no olhar da saúde coletiva. Rev Esc Enferm USP. 2007;41(n.esp):793-8.
Prevention strategies for testicular and penile cancer: an integrative review
Publication Dates
-
Publication in this collection
22 Mar 2011 -
Date of issue
Mar 2011
History
-
Received
07 May 2009 -
Accepted
22 Apr 2010