Abstract
This article discusses the resilience of the Brazilian National Health System (SUS) in the face of the COVID-19 pandemic. The analytical categories proposed by the World Health Organization were adopted to analyze the health system’s: (i) leadership and governance, (ii) financing, (iii) strategic health products, (iv) workforce, (v) health Information, and (vi) provision of services. To explore the provision of services and adapt it to the Brazilian context, we subdivided the corresponding block into five sub-blocks: (i) public health and surveillance actions, (ii) primary health care; (iii) specialized and hospital care, (iv) urgency and emergency, and (v) digital health. We conducted a non-systematic consultation of scientific literature and official documents published by Brazilian government agencies and international health organizations to obtain data related to the organization of health systems in the face of public health emergencies.
Keywords:
Brazilian National Health System; Health management; Public health emergencies
Resumo
Neste artigo, discutimos a resiliência do Sistema Único de Saúde (SUS) diante da pandemia da COVID-19. Para análise, utilizamos as categorias analíticas propostas pela Organização Mundial da Saúde (OMSOrganização Mundial da Saúde.. (2020b). Weekly Epidemiological Update: coronavirus disease 2019 (Covid-19). Recuperado de https://www.who.int/publications/m/item/weekly-epidemiological-update---3-november-2020
https://www.who.int/publications/m/item/...
) para análise de sistemas de saúde: (i) liderança e governança, (ii) financiamento, (iii) produtos estratégicos para saúde, (iv) força de trabalho, (v) informação em saúde e (vi) prestação de serviços. Para explorar a prestação de serviços e adaptá-la ao contexto brasileiro, subdividimos o bloco correspondente em 5 sub-blocos: (i) ações de saúde pública e vigilância, (ii) atenção primária em saúde; (iii) atenção especializada e hospitalar, (iv) urgência e emergência, e (v) saúde digital. Procedemos a uma consulta não sistemática à literatura científica e a documentos oficiais publicados por órgãos governamentais brasileiros e internacionais de saúde, visando obter dados relacionadas à organização de sistemas de saúde frente a emergências em saúde pública.
Palavras-chave:
Sistema Único de Saúde; Gestão em saúde; Emergências em saúde pública
Resumen
En este artículo, discutimos la resiliencia del Sistema Único de Salud (SUS) ante la pandemia de COVID-19. Para el estudio utilizamos las categorías analíticas propuestas por la Organización Mundial de la Salud (OMS) para análisis de sistemas de salud: (i) liderazgo y gobernanza, (ii) financiación, (iii) productos estratégicos para la salud, (iv) fuerza de trabajo, (v) información en salud y (vi) prestación de servicios. Para explorar la prestación de servicios y adaptarla al contexto brasileño, subdividimos el bloque correspondiente en 5 subbloques: (i) acciones de salud pública y vigilancia, (ii) atención primaria en salud; (iii) atención especializada y hospitalaria, (iv) urgencia y emergencia, y (v) salud digital. Procedemos a una consulta no sistemática a la literatura científica y a documentos oficiales publicados por órganos gubernamentales brasileños e internacionales de salud, con el objetivo de obtener datos relacionados a la organización de sistemas de salud frente a emergencias de salud pública.
Palabras clave:
Sistema Único de Salud; Gestión en salud; Emergencias en salud pública
INTRODUCTION
Initially reported in the province of Wuhan, China, in December 2019, and declared an international public health emergency by the World Health Organization (WHO) on January 30, 2020, the disease caused by the coronavirus Sars-Cov-2 (COVID- 19) affected the world in a very special way. Until November 1, 2020, with approximately 1.2 million deaths caused by the pandemic, 54% of deaths occurred in the Americas, 24% in Europe, and 12% in Asia (WHO/OMS, 2020Organização Mundial da Saúde. (2010). Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva, Switzerland: World Health Organization.). The differences in lethality among countries occurred through the interrelationship of multiple factors, but one of the decisive aspects for the quality of response to the outbreak was the resilience of health systems (Kontis, 2020Kontis, V., Bennett, J. E., Rashid, T., Parks, R. M., Pearson-Stuttard, J., Guillot, M., ... & McKee, M. (2020). Magnitude, demographics and dynamics of the effect of the first wave of the Covid-19 pandemic on all-cause mortality in 21 industrialized countries. Nature Medicine, 26, 1919-1928.).
The analysis of health systems’ resilience has received increasing attention from global health. The abrupt reduction in financial resources for the area, caused by economic crises and fiscal austerity measures, and by the rapid increase in healthcare demand, motivated by epidemics, natural disasters, and the arrival of a large number of refugees, has produced shocks on health systems more frequently (Thomas et al., 2020Thomas, S., Sagan, A., Larkin, J., Cylus, J., Figueras, J., & Karanikolos, M. (2020). Policy brief. In S. Thomas, A. Sagan, J. Larkin, J. Cylus, J. Figueras, & M. Karanikolos (Eds), Strengthening health systems resilience: key concepts and strategies. Copenhagen, Denmark: World Health Organization; European Observatory on Health Systems and Policies.). The resilience analysis seeks to understand the capacity of health agents, institutions, and populations to prepare themselves to respond to such shocks, keeping the systems’ essential functions without changing health outcomes, as well as the ability to reorganize from lessons learned (Kruk et al., 2017Kruk, M. E., Ling, E J, Bitton, A., Cammett, M., Cavanaugh, K., Chopra, M., ... Marten, R. (2017). Building resilient health systems: a proposal for a resilience index. BMJ Global Health, 357, j2323.).
In general, countries with weaknesses in structuring points of health systems show less resilience to shocks that can lead to the collapse of essential services, affecting groups or the whole population (Kruk et al., 2017Kruk, M. E., Ling, E J, Bitton, A., Cammett, M., Cavanaugh, K., Chopra, M., ... Marten, R. (2017). Building resilient health systems: a proposal for a resilience index. BMJ Global Health, 357, j2323.). In COVID-19, however, even countries with well-structured health systems collapsed, due to the rapid increase of the demand for hospitalizations in Intensive Care Units (ICU) (Legido-Quigley et al., 2020Legido-Quigley, H., Asgari, N., Teo, Y. Y., Leung, G. M., Oshitani, H., Fukuda, K., … Heymann D. (2020) Are high-performing health systems resilient against the Covid-19 epidemic? The Lancet, 395(10227), 848-850.). In addition to the direct impact of the disease, the pandemic has also caused several side effects on the systems and population health (Roberton et al., 2020Roberton, T., Carter, E. D., Chou, V. B., Stegmuller, A. R., Jackson, B. D., Tam, Y., ... Walker, N. (2020). Early estimates of the indirect effects of the Covid-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. The Lancet Global Health, 8(7), E901-E908.).
The crowding of services with suspected cases of COVID-19, and the fear of searching formal health facilities for the control of chronic diseases have worsened pre-existing conditions (Rezende, Thome, Schveitzer, Souza, & Szwarcwald, 2020Rezende, L. F. M., Thome, B., Schveitzer, M. C., Souza, P. R. B Jr.., , & Szwarcwald, C. L. (2020). Adults at high-risk of severe coronavirus disease-2019 (Covid-19) in Brazil. Revista de Saúde Pública, 54, 1-9.). There was also an increase in psychosocial problems, such as domestic violence, among the population (Vieira, Garcia & Maciel, 2020Vieira, P. R., Garcia, L. P, & Maciel, E. L. N. (2020). Isolamento social e o aumento da violência doméstica: o que isso nos revela? Revista Brasileira de Epidemiologia,23, e200033.), and of mental health, among health professionals who deal directly with patients’ care (Lai et al., 2020Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., ... Tan, H. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. Jama Network Open, 3(3), e203976-e203976.), and in the population (Pfefferbaum & North, 2020Pfefferbaum, B., & North, C. S. (2020). Mental health and the Covid-19 pandemic. New England Journal of Medicine, 383(6), 510-512.). In addition, in countries with large socioeconomic inequalities and fragile social security systems, population groups in worse economic conditions were more exposed to virus contamination and had more difficulty in accessing diagnostic and therapeutic services, hindering the control of disease transmission (F. Ahmed, N. Ahmed, Pissarides & Stiglitz, 2020Ahmed, F., Ahmed, N. E., Pissarides, C., & Stiglitz, J. (2020). Why inequality could spread Covid-19. The Lancet Public Health, 5(5), e240.).
Despite having a universal health system, and having created a response system to public health emergencies, Brazil has the second highest number of deaths caused by the disease, with more than 160 thousand deaths recorded between March and November 2020 (OMS, 2020Organização Mundial da Saúde. (2010). Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva, Switzerland: World Health Organization.). Given this situation, it is of great importance to analyze how the Brazilian health system has responded to the pandemic. In this study, we present a brief analysis of the resilience of the Brazilian National Health System (SUS) in the face of the COVID-19 pandemic.
METHODS
To analyze the resilience of SUS before the pandemic, we used the model proposed by WHO (OMS, 2010Organização Mundial da Saúde. (2010). Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva, Switzerland: World Health Organization.) as a reference, with six building blocks.
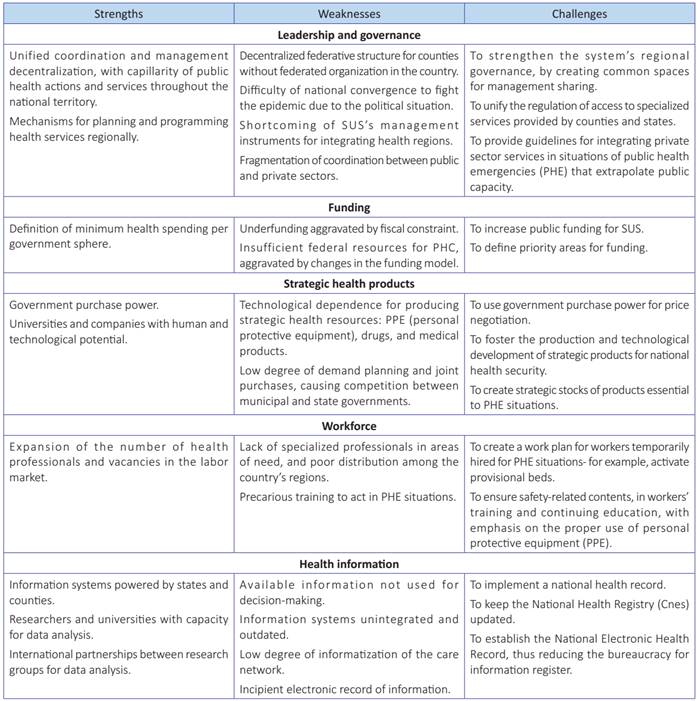
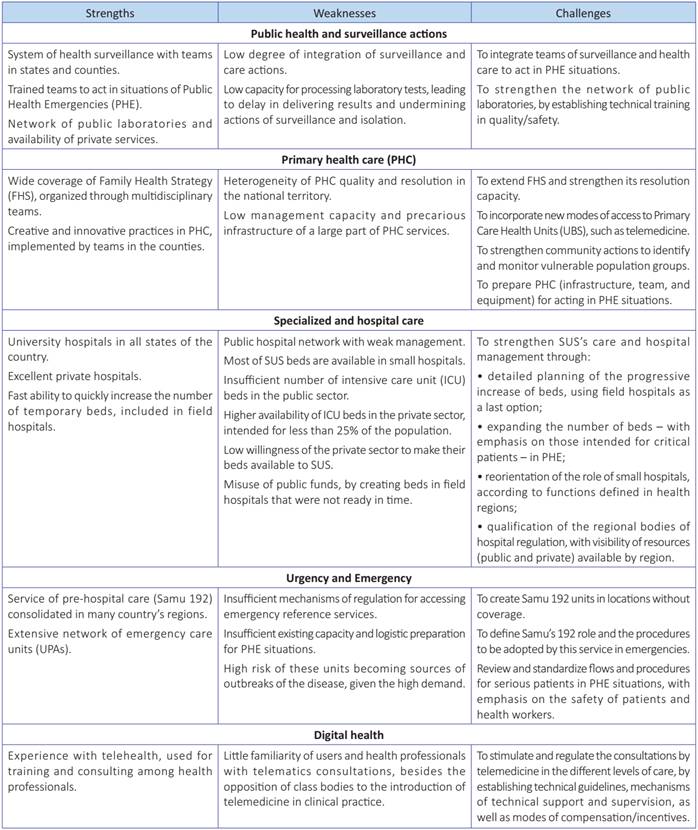
According to this model, to accomplish their functions, health systems need to have (i) leadership and governance, (ii) funding, (iii) strategic health products, (iv) workforce, (v) health information, and (vi) service provision. To explore the provision of services and adapt it to the Brazilian context, we subdivided this item into five sub-blocks: (i) public health and surveillance actions, (ii) primary health care; (iii) specialized and hospital care, (iv) urgency and emergency, and (v) digital health.
We carried out a non-systematic survey of scientific literature and official documents published by Brazilian and international government health bodies, as well as experts, in order to get data related to the organization of health systems in the face of public health emergencies. Then, we conducted a simple qualitative analysis, seeking to classify strengths, weaknesses, and challenges in SUS’s structure and organization that affect the pandemic.
RESULTS AND DISCUSSION
We arranged the results in Boxes 1 and 2. The first box presents strengths, weaknesses, and challenges related to (i) leadership and governance, (ii) funding, (iii) strategic health products, (iv) workforce, and (v) health information.
Box 2shows strengths, weaknesses, and challenges of SUS’s structure and organization, regarding service provision, divided in sub-blocks.
STRENGTHS AND WEAKNESSES
A health system with SUS’s characteristics should be a powerfull tool for fighting COVID-19 pandemic (Croda et al., 2020Croda, J., Oliveira, W. K. D., Frutuoso, R. L., Mandetta, L. H., Baia-da-Silva, D. C., Brito-Sousa, J. D., ... Lacerda, M. V. G. (2020). Covid-19 in Brazil: advantages of a socialized unified health system and preparation to contain cases. Revista da Sociedade Brasileira de Medicina Tropical, 53, e20200167.). The country has structured a reasonable response chain to public health emergencies (PHE), which was used successfully in tackling epidemics such as H1N1, dengue and zika, in natural disasters, and in support of major sports events, like the FIFA World Cup and the Olympic Games (Teixeira, Costa, Carmo, Oliveira & Penna, 2018Teixeira, M. G., Costa, M. D., Carmo, E. H., Oliveira, W. K., & Penna, G. O. (2018). Vigilância em saúde no SUS: construção, efeitos e perspectivas. Ciência & Saúde Coletiva, 23, 1811-8.). However, SUS’s implementation was incomplete, and its structural problems were aggravated by fiscal austerity measures and recent policies adopted by the federal government (Castro et al., 2020Castro, M. C., Massuda, A., Almeida, G., Menezes-Filho, N. A., Andrade, M. V., Noronha, K. V. M. de S., ... Giovanella, L. (2019). Brazil’s unified health system: the first 30 years and prospects for the future. The Lancet, 394(10195), 345-356.). Therefore, Brazil faced the pandemic with a fragile SUS and with less resilience than it should have.
Internationally recognized for the success of programs that contributed to expand the care network, increase access to services, and improve health indicators, decentralization to the municipal level allowed providing capillarity to SUS’s management and structuring a network of public health services throughout the country (Viacava, Oliveira, Carvalho, Laguardia & Bellido, 2018Viacava, F., Oliveira, R. A., Carvalho, C. D., Laguardia, J., & Bellido, J. G. (2018). SUS: oferta, acesso e utilização de serviços de saúde nos últimos 30 anos. Ciência & Saúde Coletiva, 23, 1751-62.). In each Brazilian county, there is a health department and technical teams, even if they have different qualifications.
However, the fragile governance of the health system in 2020, crucial for coordinating the response to the epidemic (Organization for Economic Cooperation and Development [OECD], 2020Organização para a Cooperação e o Desenvolvimento Econômico. (2020). OECD Policy Responses to Coronavirus (Covid-19). Building resilience to the Covid-19 pandemic: the role of centres of government. Recuperado de https://read.oecd-ilibrary.org/view/?ref=135_135808-q2mj1rudey&title=Building-resilience-to-the-Covid-19-pandemic-the-role-of-centres-of-government
https://read.oecd-ilibrary.org/view/?ref...
), can be seen at the national level, but also in many states and counties (Sodré, 2020Sodré, F. (2020). Epidemia de Covid-19: questões críticas para a gestão da saúde pública no Brasil. Trabalho, Educação e Saúde, 18(3), e00302134.). In part, this is due to the situation; the extended political crisis prevented building a minimum convergence to address, among others, the country’s health problems (Abrucio, 2020Abrucio, F. L, Grin, E. J., Franzese, C., Segatto, C. I., & Couto, C. G. (2020). Combate à Covid-19 sob o federalismo bolsonarista: um caso de descoordenação intergovernamental. Revista de Administração Pública, 54(4), 663-677).
Initial efforts from the Ministry of Health to communicate the pandemic risks to the population, and to keep physical distance and wear masks, had a positive effect. Most of the states adopted measures for social distancing (Silva et al., 2020Silva, L. L. S. D., Lima, A. F. R., Polli, D. A., Razia, P. F. S., Pavão, L. F. A., Cavalcanti, M. A. F. D. H. ... Toscano, C. M. (2020). Medidas de distanciamento social para o enfrentamento da Covid-19 no Brasil: caracterização e análise epidemiológica por estado. Cadernos de Saúde Pública, 36, e00185020.), and a good part of the population changed habits, making use of gel alcohol for cleaning hands and protective masks (Lima-Costa, Mambrini, Andrade, Peixoto & Macinko, 2020Lima-Costa, M. F., Mambrini, J. V. D. M., Andrade, F. B. D., Peixoto, S. W. V., & Macinko, J. (2020). Distanciamento social, uso de máscaras e higienização das mãos entre participantes do Estudo Longitudinal da Saúde dos Idosos Brasileiros: iniciativa Elsi-Covid-19. Cadernos de Saúde Pública, 36, e00193920.). However, health guidelines stumbled over the position and attitudes of the President of the Republic, who, under the argument of protecting the economy, contradicted the recommendations of social distance, passed on fake news about COVID-19, and defended the use of chloroquine as the main strategy for fighting the disease (Lancet, 2020Lancet, T. (2020). Covid-19 in Brazil: “So what?”. The Lancet, 395(10235), 1461.).
The conflict with the president over the guidelines for preventing the virus transmission resulted in the dismissal of the Minister of Health, and of a second minister, less than a month after his inauguration. The Army general, who temporarily took over the Ministry, militarized it and later became effective in office. There were also some situations of conflict between the minister and the president, regarding the purchase of vaccines.
Although cyclical problems affected the response capacity, the current federative model also represented a more serious structural problem for SUS. The municipal authority model of organization, which provided capillarity to management and the creation of a basic health network, was an impediment for implementing complex services, which were concentrated in a few urban centers, and in the private sector (Albuquerque, Cesse, Felisberto, Samico & Frias, 2019Albuquerque, A. C. D., Cesse, E. A. P., Felisberto, E., Samico, I. C., & Frias, P. G. D. (2019). Avaliação de desempenho da regionalização da vigilância em saúde em seis regiões de saúde brasileiras. Cadernos de Saúde Pública, 35, e00065218.). Instruments established at SUS, such as inter-management commissions and consortia, were insufficient to integrate municipal and state care networks in health regions, which often led to the duplication of lines for accessing services and to the waste of scarce resources (Viana, Bousquat, Melo & Medina, 2018Viana, A. L. D., Bousquat, A., Melo, G. A., De Negri, A Filho., & Medina, M. G. (2018). Regionalização e redes de saúde. Ciência & Saúde Coletiva, 23, 1791-1798.).
Another structural problem of SUS is public underfunding. Despite the definition of a minimum health spending by government level, Brazil is the only country with a universal health system where private health spending is higher than public: 58% of the total (Instituto Brasileiro de Geografia e Estatística [IBGE], 2019Instituto de Comunicação e Informação Científica e Tecnológica em Saúde. (2020). MonitoraCovid-19. Recuperado de https://bigdata-covid19.icict.fiocruz.br/
https://bigdata-covid19.icict.fiocruz.br...
). Since 2015, fiscal restrictions have compromised federal health resources (Massuda, Hone, Leles, Castro & Atun, 2018Massuda, A., Hone, T., Leles, F. A. G., Castro, M. C., & Atun, R. (2018). The Brazilian health system at crossroads: progress, crisis and resilience. BMJ Global Health, 3(4), e000829.).
With regard to strategic health products, the country has an important government purchasing power (Fonseca & Costa, 2015Fonseca, E. M. D., & Costa, N. D. R. (2015). Federalismo, complexo econômico-industrial da saúde e assistência farmacêutica de alto custo no Brasil.Ciência & Saúde Coletiva,20, 1165-1176.). Despite that, universities and companies with human and technological potential, like Oswaldo Cruz Foundation (Fiocruz) and Butantan Institute, which established research partnerships with international laboratories for the development and production of vaccines against the new coronavirus, suffer the lack of basic products, which is still one of the main weaknesses in fighting COVID-19. Part of the shortage of inputs is due to national technological dependence, since industrial production has moved to countries with cheap labor and a less demanding environmental legislation. However, this is also a consequence of vaccines in purchase management, in the articulation of joint acquisitions between states and counties, and in keeping security stocks (Monteiro, 2020Monteiro, N. (2020). O Estado em desmonte frente à epidemia da Covid-19. Physis - Revista de Saúde Coletiva, 30, e300304.).
The pandemic also highlights problems related to the workforce. Despite the increase in the number of health professionals and vacancies in the Brazilian labor market since SUS’s creation, its imbalanced distribution across regions causes shortcoming of specialized professionals in the system’s different areas (Scheffer, 2018Scheffer, M. (2018). Demografia médica no Brasil São Paulo, SP: FMUSP, CFM.). COVID-19 also revealed a precarious preparation and training of professionals to act in PHE situations. Lotta, Dossiatti, Magri, Corrêa and Beck (2020Lotta, G., Dossiatti, D., Magri, G., Corrêa, M., & Beck, A. (2020). A pandemia de Covid-19 e os profissionais de saúde pública no Brasil. São Paulo, SP: Fundação Getulio Vargas, Núcleo de Estudos da Burocracia) observed that only a third of health professionals had appropriate PPE during the epidemic, and only 20% received training on its correct use. Four out of five interviewed professionals were afraid of catching the virus, and only 15% felt prepared for work.
The availability of reliable information is another critical aspect in the preparation and response to the disease (OMS, 2020Organização Mundial da Saúde. (2010). Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva, Switzerland: World Health Organization.). Despite SUS having different systems that generate a wide list of health information at the local level (Pinto, Freitas & Figueiredo, 2018Pinto, L. F., Freitas, M. P. S. D., & Figueiredo, A. W. S. A. D. (2018). Sistemas Nacionais de Informação e levantamentos populacionais: algumas contribuições do Ministério da Saúde e do IBGE para a análise das capitais brasileiras nos últimos 30 anos. Ciência & Saúde Coletiva, 23, 1859-1870.), the low degree of informatization of the care network, the incipient use of electronic health records, and problems for integrating and updating databases hinder care information for decision-making (Jorge, Laurenti & Gotlieb, 2010Jorge, M. H. P. M., Laurenti, R., & Gotlieb, S. L. D. (2010). Avaliação dos sistemas de informação em saúde no Brasil. Cadernos Saúde Coletiva, 18(1), 7-18.).
On the other hand, there are initiatives developed by Brazilian researchers and universities, such as Fiocruz ‘Monitora COVID’ and the researchers’ network of the Observatory COVID-19 BR. In addition, there is an unprecedented consortium of press bodies. All of them have provided information in real time on the evolution of the disease in the country. This was an important counterpoint to potential attempts to delay or distort official data.
Regarding service provision, SUS enabled the creation of a national and decentralized health surveillance system, composed of teams that work in the prevention and control of diseases and in the preparation of contingency plans for PHE (Teixeira et al., 2018Teixeira, M. G., Costa, M. D., Carmo, E. H., Oliveira, W. K., & Penna, G. O. (2018). Vigilância em saúde no SUS: construção, efeitos e perspectivas. Ciência & Saúde Coletiva, 23, 1811-8.). However, when facing COVID-19, the shortage of laboratory tests and the lack of clinical criteria for diagnostic confirmation led to underreporting of cases, which interfered in the ability to analyze and make decisions according to local, regional, and national epidemiological situations (Magno et al., 2020Magno, L., Rossi, T A, Mendonça-Lima, F. W., Santos, C. C., Campos, G. B., Marques, L. M., ... Dourado I. (2020). Desafios e propostas para ampliação da testagem e diagnóstico para Covid-19 no Brasil. Ciência & Saúde Coletiva, 25, 3355-64.).
Finally, the expansion of the care network that took place at SUS expanded PHC coverage and access to emergency services. However, in hospital and specialized care, despite the existence of federal university hospitals in all states, the distribution of ICU beds is concentrated in a few urban centers and in private hospitals, some of them excellent (Carpanez & Malik, 2019Carpanez, L. R., & Malik, A. M. (2019, julho). O efeito da municipalização no sistema hospitalar brasileiro: os hospitais de pequeno porte. Ciência & Saúde Coletiva. Recuperado de http://www.cienciaesaudecoletiva.com.br/artigos/o-efeito-da-municipalizacao-no-sistema-hospitalar-brasileiro-os-hospitais-de-pequeno-porte/17293
http://www.cienciaesaudecoletiva.com.br/...
). Before the pandemic, 70% of the Brazilian health regions did not have the minimum number of beds per inhabitant recommended in a normal situation (Rache et al., 2020Rache, B., Rocha, R., Nunes, L., Spinola, P., Malik, A. M., & Massuda, A. (2020, março). Necessidades de infraestrutura do SUS em preparo à Covid-19: leitos de UTI, respiradores e ocupação hospitalar (Nota Técnica nº 3). Rio de Janeiro, RJ: Instituto de Estudos para Políticas de Saúde.).
In addition the inequity, the heterogeneous quality of the provided services, the precarious capacity to coordinate the care network, and fraud in private service contracting are substantial weaknesses in fighting the pandemic (Florêncio & Zanon, 2020Florêncio, M. A Filho, & Zanon, P. B. (2020). Covid-19 e corrupção: políticas de controle em face às medidas emergenciais. Revista Pensamento Jurídico, 14(2), 25-47.). Remote access to health, which could be an alternative to expand entrance into the system, is restricted, due to little tradition in digital health, used only for training and technical consulting activities, in addition to legal constraints.
CHALLENGES
The success of some countries in fighting the epidemic shows that, in addition to governments’ efficient action and society’s engagement, it is essential to rely on a good health system. Such a system must have an appropriate governance, robust information systems to support decision, health professionals specialized in different areas, and technological and care infrastructure, suitable for carrying out actions for prevention, treatment, and recovery (Sachs et al., 2020Sachs, J. D., Karim, S. A., Aknin, L., Allen, J., Brosbøl, K., Barron, G. C., ... & Haines, A. (2020). Lancet Covid-19 Commission Statement on the occasion of the 75th session of the UN General Assembly. The Lancet, 396(10257), 1102-1124.).
In Brazil, one of the main post-COVID-19 challenges will be to strengthen SUS and correct its structural flaws. First, it will be necessary to create a regional governance in the health system, with spaces for sharing management and responsible for unifying the regulation of access to specialized services provided by counties and states, as is the case with transplants. In addition, it is required to create guidelines for better use of resources available in the private sector, when SUS’ capacity is exceeded (Massuda, Tasca & Malik, 2020Massuda, A., Tasca, R., & Malik, A. M. (2020). Uso de leitos hospitalares privados por sistemas públicos de saúde na resposta à Covid-19. Preprint Scielo. Recuperado dehttps://preprints.scielo.org/index.php/scielo/preprint/view/1320
https://preprints.scielo.org/index.php/s...
).
Second, to address the problem of public underfunding and expansion of the capacity to direct resources to priority areas of the health system, including PHC, health surveillance, strategic health products, and specialized areas of greatest need.
Third, to improve the provision of strategic health products and use government’s purchasing power, both for price negotiation and to foster the production and technological development of items relevant for national health security.
Fourth, SUS’s strengthening depends on a policy for appropriate training and distribution of the workforce in the system’s areas of need. It is necessary to create a plan for hiring temporary workers during emergencies, and to ensure, in the formative, and in continuing and permanent education of professionals, contents related to acting in PHE, emphasizing, for example, the proper use of PPE.
Fifth, the quality of SUS’s management depends on the availability of timely, reliable, and updated information. To this end, it is urgent to improve information systems, integrate databases, and reduce the bureaucracy for entering data, thus avoiding duplication. Information should also be transparent and easily accessible, with an emphasis on fighting fake news.
Finally, COVID-19 is likely to change substantially the way we provide services. Strengthening surveillance systems and integrating them to care is crucial for SUS’s better performance outside PHE situations. In PHC, in addition to clinical quality, it is essential to strengthen community actions, seeking to identify and monitor more vulnerable population groups. Telemedicine service, at different levels of care, should be part of the routine of health systems, and will require technical guidelines, supervision, technical support, and compensation mechanisms.
In hospital care, Brazil will need a policy to address the inequity in the distribution of ICU beds among country’s regions, and the quality of the services provided. In PHE situations, such as the pandemic, it is essential to adopt measures for the progressive expansion of beds, reorientation of small hospitals’ activity - with functions defined within the scope of health care networks - and qualification of the regional technical bodies for care regulation. In addition, to take more advantage of the excellent university and private hospitals.
CONCLUSION
Fighting COVID-19 exposed SUS’s strengths and weaknesses. On the one hand, the importance of a universal, comprehensive, and free health system was recognized in an unprecedented way in Brazil. On the other hand, its weaknesses, aggravated by the political and economic crisis and the federal government conduct, have also never been more evident. The pandemic also showed that resilient health systems are essential not just for ensuring the right to health, but also for keeping social and economic activities. Certainly, countries that have been successful in facing the disease will be best positioned for returning to social and economic activities, even if normality is restored only after vaccination of the population. In a post-COVID-19 scenario, strengthening SUS and improving its management must be on the agenda of health and other sectors of society.
REFERÊNCIAS
- Abrucio, F. L, Grin, E. J., Franzese, C., Segatto, C. I., & Couto, C. G. (2020). Combate à Covid-19 sob o federalismo bolsonarista: um caso de descoordenação intergovernamental. Revista de Administração Pública, 54(4), 663-677
- Ahmed, F., Ahmed, N. E., Pissarides, C., & Stiglitz, J. (2020). Why inequality could spread Covid-19. The Lancet Public Health, 5(5), e240.
- Albuquerque, A. C. D., Cesse, E. A. P., Felisberto, E., Samico, I. C., & Frias, P. G. D. (2019). Avaliação de desempenho da regionalização da vigilância em saúde em seis regiões de saúde brasileiras. Cadernos de Saúde Pública, 35, e00065218.
- Carpanez, L. R., & Malik, A. M. (2019, julho). O efeito da municipalização no sistema hospitalar brasileiro: os hospitais de pequeno porte. Ciência & Saúde Coletiva Recuperado de http://www.cienciaesaudecoletiva.com.br/artigos/o-efeito-da-municipalizacao-no-sistema-hospitalar-brasileiro-os-hospitais-de-pequeno-porte/17293
» http://www.cienciaesaudecoletiva.com.br/artigos/o-efeito-da-municipalizacao-no-sistema-hospitalar-brasileiro-os-hospitais-de-pequeno-porte/17293 - Castro, M. C., Massuda, A., Almeida, G., Menezes-Filho, N. A., Andrade, M. V., Noronha, K. V. M. de S., ... Giovanella, L. (2019). Brazil’s unified health system: the first 30 years and prospects for the future. The Lancet, 394(10195), 345-356.
- Croda, J., Oliveira, W. K. D., Frutuoso, R. L., Mandetta, L. H., Baia-da-Silva, D. C., Brito-Sousa, J. D., ... Lacerda, M. V. G. (2020). Covid-19 in Brazil: advantages of a socialized unified health system and preparation to contain cases. Revista da Sociedade Brasileira de Medicina Tropical, 53, e20200167.
- Fonseca, E. M. D., & Costa, N. D. R. (2015). Federalismo, complexo econômico-industrial da saúde e assistência farmacêutica de alto custo no Brasil.Ciência & Saúde Coletiva,20, 1165-1176.
- Florêncio, M. A Filho, & Zanon, P. B. (2020). Covid-19 e corrupção: políticas de controle em face às medidas emergenciais. Revista Pensamento Jurídico, 14(2), 25-47.
- Instituto Brasileiro de Geografia e Estatística. (2019). Contas Nacionais número 71 - Conta-Satélite de Saúde 2010-2017. Recuperado de https://biblioteca.ibge.gov.br/visualizacao/livros/liv101690_notas_tecnicas.pdf
» https://biblioteca.ibge.gov.br/visualizacao/livros/liv101690_notas_tecnicas.pdf - Instituto de Comunicação e Informação Científica e Tecnológica em Saúde. (2020). MonitoraCovid-19 Recuperado de https://bigdata-covid19.icict.fiocruz.br/
» https://bigdata-covid19.icict.fiocruz.br/ - Jorge, M. H. P. M., Laurenti, R., & Gotlieb, S. L. D. (2010). Avaliação dos sistemas de informação em saúde no Brasil. Cadernos Saúde Coletiva, 18(1), 7-18.
- Kontis, V., Bennett, J. E., Rashid, T., Parks, R. M., Pearson-Stuttard, J., Guillot, M., ... & McKee, M. (2020). Magnitude, demographics and dynamics of the effect of the first wave of the Covid-19 pandemic on all-cause mortality in 21 industrialized countries. Nature Medicine, 26, 1919-1928.
- Kruk, M. E., Ling, E J, Bitton, A., Cammett, M., Cavanaugh, K., Chopra, M., ... Marten, R. (2017). Building resilient health systems: a proposal for a resilience index. BMJ Global Health, 357, j2323.
- Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., ... Tan, H. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. Jama Network Open, 3(3), e203976-e203976.
- Lancet, T. (2020). Covid-19 in Brazil: “So what?”. The Lancet, 395(10235), 1461.
- Legido-Quigley, H., Asgari, N., Teo, Y. Y., Leung, G. M., Oshitani, H., Fukuda, K., … Heymann D. (2020) Are high-performing health systems resilient against the Covid-19 epidemic? The Lancet, 395(10227), 848-850.
- Lima-Costa, M. F., Mambrini, J. V. D. M., Andrade, F. B. D., Peixoto, S. W. V., & Macinko, J. (2020). Distanciamento social, uso de máscaras e higienização das mãos entre participantes do Estudo Longitudinal da Saúde dos Idosos Brasileiros: iniciativa Elsi-Covid-19. Cadernos de Saúde Pública, 36, e00193920.
- Lotta, G., Dossiatti, D., Magri, G., Corrêa, M., & Beck, A. (2020). A pandemia de Covid-19 e os profissionais de saúde pública no Brasil São Paulo, SP: Fundação Getulio Vargas, Núcleo de Estudos da Burocracia
- Magno, L., Rossi, T A, Mendonça-Lima, F. W., Santos, C. C., Campos, G. B., Marques, L. M., ... Dourado I. (2020). Desafios e propostas para ampliação da testagem e diagnóstico para Covid-19 no Brasil. Ciência & Saúde Coletiva, 25, 3355-64.
- Massuda, A., Hone, T., Leles, F. A. G., Castro, M. C., & Atun, R. (2018). The Brazilian health system at crossroads: progress, crisis and resilience. BMJ Global Health, 3(4), e000829.
- Massuda, A., Tasca, R., & Malik, A. M. (2020). Uso de leitos hospitalares privados por sistemas públicos de saúde na resposta à Covid-19. Preprint Scielo Recuperado dehttps://preprints.scielo.org/index.php/scielo/preprint/view/1320
» https://preprints.scielo.org/index.php/scielo/preprint/view/1320 - Monteiro, N. (2020). O Estado em desmonte frente à epidemia da Covid-19. Physis - Revista de Saúde Coletiva, 30, e300304.
- Observatório COVID-19 BR. (2020). Explore o Observatório Recuperado dehttps://covid19br.github.io/
» https://covid19br.github.io/ - Organização Mundial da Saúde. (2010). Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies Geneva, Switzerland: World Health Organization.
- Organização Mundial da Saúde. (2020a). Critical preparedness, readiness and response actions for Covid-19: interim guidance Geneva, Switzerland: World Health Organization.
- Organização Mundial da Saúde.. (2020b). Weekly Epidemiological Update: coronavirus disease 2019 (Covid-19) Recuperado de https://www.who.int/publications/m/item/weekly-epidemiological-update---3-november-2020
» https://www.who.int/publications/m/item/weekly-epidemiological-update---3-november-2020 - Organização para a Cooperação e o Desenvolvimento Econômico. (2020). OECD Policy Responses to Coronavirus (Covid-19). Building resilience to the Covid-19 pandemic: the role of centres of government Recuperado de https://read.oecd-ilibrary.org/view/?ref=135_135808-q2mj1rudey&title=Building-resilience-to-the-Covid-19-pandemic-the-role-of-centres-of-government
» https://read.oecd-ilibrary.org/view/?ref=135_135808-q2mj1rudey&title=Building-resilience-to-the-Covid-19-pandemic-the-role-of-centres-of-government - Pfefferbaum, B., & North, C. S. (2020). Mental health and the Covid-19 pandemic. New England Journal of Medicine, 383(6), 510-512.
- Pinto, L. F., Freitas, M. P. S. D., & Figueiredo, A. W. S. A. D. (2018). Sistemas Nacionais de Informação e levantamentos populacionais: algumas contribuições do Ministério da Saúde e do IBGE para a análise das capitais brasileiras nos últimos 30 anos. Ciência & Saúde Coletiva, 23, 1859-1870.
- Rache, B., Rocha, R., Nunes, L., Spinola, P., Malik, A. M., & Massuda, A. (2020, março). Necessidades de infraestrutura do SUS em preparo à Covid-19: leitos de UTI, respiradores e ocupação hospitalar (Nota Técnica nº 3). Rio de Janeiro, RJ: Instituto de Estudos para Políticas de Saúde.
- Remuzzi, A., & Remuzzi, G. (2020). Covid-19 and Italy: what next? The Lancet, 395(10231), 1225-1228.
- Rezende, L. F. M., Thome, B., Schveitzer, M. C., Souza, P. R. B Jr.., , & Szwarcwald, C. L. (2020). Adults at high-risk of severe coronavirus disease-2019 (Covid-19) in Brazil. Revista de Saúde Pública, 54, 1-9.
- Roberton, T., Carter, E. D., Chou, V. B., Stegmuller, A. R., Jackson, B. D., Tam, Y., ... Walker, N. (2020). Early estimates of the indirect effects of the Covid-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. The Lancet Global Health, 8(7), E901-E908.
- Sachs, J. D., Karim, S. A., Aknin, L., Allen, J., Brosbøl, K., Barron, G. C., ... & Haines, A. (2020). Lancet Covid-19 Commission Statement on the occasion of the 75th session of the UN General Assembly. The Lancet, 396(10257), 1102-1124.
- Scheffer, M. (2018). Demografia médica no Brasil São Paulo, SP: FMUSP, CFM.
- Silva, L. L. S. D., Lima, A. F. R., Polli, D. A., Razia, P. F. S., Pavão, L. F. A., Cavalcanti, M. A. F. D. H. ... Toscano, C. M. (2020). Medidas de distanciamento social para o enfrentamento da Covid-19 no Brasil: caracterização e análise epidemiológica por estado. Cadernos de Saúde Pública, 36, e00185020.
- Sodré, F. (2020). Epidemia de Covid-19: questões críticas para a gestão da saúde pública no Brasil. Trabalho, Educação e Saúde, 18(3), e00302134.
- Teixeira, M. G., Costa, M. D., Carmo, E. H., Oliveira, W. K., & Penna, G. O. (2018). Vigilância em saúde no SUS: construção, efeitos e perspectivas. Ciência & Saúde Coletiva, 23, 1811-8.
- Thomas, S., Sagan, A., Larkin, J., Cylus, J., Figueras, J., & Karanikolos, M. (2020). Policy brief. In S. Thomas, A. Sagan, J. Larkin, J. Cylus, J. Figueras, & M. Karanikolos (Eds), Strengthening health systems resilience: key concepts and strategies Copenhagen, Denmark: World Health Organization; European Observatory on Health Systems and Policies.
- Viacava, F., Oliveira, R. A., Carvalho, C. D., Laguardia, J., & Bellido, J. G. (2018). SUS: oferta, acesso e utilização de serviços de saúde nos últimos 30 anos. Ciência & Saúde Coletiva, 23, 1751-62.
- Viana, A. L. D., Bousquat, A., Melo, G. A., De Negri, A Filho., & Medina, M. G. (2018). Regionalização e redes de saúde. Ciência & Saúde Coletiva, 23, 1791-1798.
- Vieira, P. R., Garcia, L. P, & Maciel, E. L. N. (2020). Isolamento social e o aumento da violência doméstica: o que isso nos revela? Revista Brasileira de Epidemiologia,23, e200033.
-
[Translated version] Note: All quotes in English translated by this article’s translator.
Publication Dates
-
Publication in this collection
20 Dec 2021 -
Date of issue
Nov 2021
History
-
Received
24 Aug 2020 -
Accepted
18 Dec 2020




 Source: Elaborated by the authors.
Source: Elaborated by the authors.
 Source: Elaborated by the authors.
Source: Elaborated by the authors.