Abstracts
Objective:
to compare clinical and cost effectiveness of midazolam and diazepam for urgent intubation.
Methods:
patients admitted to the Central ICU of the Santa Casa Hospital Complex in Porto Alegre, over the age of 18 years, undergoing urgent intubation during 6 months were eligible. Patients were randomized in a single-blinded manner to either intravenous diazepam or midazolam. Diazepam was given as a 5 mg intravenous bolus followed by aliquots of 5 mg each minute. Midazolam was given as an intravenous bolus of 5 mg with further aliquots of 2.5 mg each minute. Ramsay sedation scale 5-6 was considered adequate sedation. We recorded time and required doses to reach adequate sedation and duration of sedation.
Results:
thirty four patients were randomized, but one patient in the diazepam group was excluded because data were lost. Both groups were similar in terms of illness severity and demographics. Time for adequate sedation was shorter (132 ± 87 sec vs. 224 ± 117 sec, p = 0.016) but duration of sedation was similar (86 ± 67 min vs. 88 ± 50 min, p = 0.936) for diazepam in comparison to midazolam. Total drug dose to reach adequate sedation after either drugs was similar (10.0 [10.0-12.5] mg vs. 15.0 [10.0-17.5] mg, p = 0.248). Arterial pressure and sedation intensity reduced similarly overtime with both drugs. Cost of sedation was lower for diazepam than for midazolam (1.4[1.4-1.8] vs. 13.9[9.4-16.2] reais, p <0.001).
Conclusions:
intubation using intravenous diazepam and midazolam is effective and well tolerated. Sedation with diazepam is associated to a quicker sedation time and to lower costs.
deep sedation; drug costs; intubation; randomized controlled trial; diazepam; midazolam
Objetivo:
comparar eficácia clínica e custo de midazolam e diazepam para intubação urgente.
Métodos:
pacientes internados na UTI Central do Complexo Hospitalar Santa Casa de Porto Alegre, >18 anos de idade e submetidos a entubação urgente durante seis meses eram elegíveis. Pacientes foram randomizados para receber diazepam ou midazolam intravenoso. Diazepam foi dado como bolus IV de 5 mg seguido por alíquotas de 5 mg a cada minuto. Midazolam foi dado como um bolus IV de 5 mg, com alíquotas adicionais de 2,5 mg a cada minuto. Escala de sedação de Ramsay 5-6 foi considerada sedação adequada. Registramos tempo e doses necessárias para atingir sedação adequada e sua duração.
Resultados:
trinta e quatro pacientes foram randomizados; um paciente no grupo diazepam foi excluído por perda dos dados. Grupos foram semelhantes para gravidade da doença e demografia. Tempo de sedação adequada foi mais curto (132 ± 87 vs. 224 ± 117 segundos, p = 0,016), mas a duração da sedação foi similar (86 ± 67 vs. 88 ± 50 min., p = 0,936) para o diazepam em comparação com o midazolam. Dose total da droga para atingir a sedação adequada foi semelhante para ambas as drogas (10,0 [10,0-12,5] vs. 15,0 [10,0-17,5] mg, p = 0,248). Pressão arterial e intensidade da sedação reduziram da mesma forma para ambas as drogas ao longo do tempo. O custo da sedação foi menor para diazepam do que para midazolam (1,4[1,4-1,8] vs. 13,9[9,4-16,2] reais, p < 0,001).
Conclusões:
entubação usando diazepam e midazolam intravenosos é eficaz e bem tolerada. Sedação com diazepam está associada a sedação mais rápida e menores custos.
sedação profunda; entubação; diazepam; midazolam; ensaio clínico controlado aleatório; custos de medicamentos
Introduction
When physicians around the world started using diazepam in the 1960s, numerous studies
were published showing that intravenous diazepam as sole sedative agent was safe, easy
to use and well tolerated by patients.11 Kahler RL, Burrow GN, Felig P. Diazepam-induced amnesia for
cardioversion. JAMA 1967; 200:997-998.
2 Nutter DO, Massumi RA. Diazepam in cardioversion. N Engl J Med 1965;
273(12):650-651.
3 Lebowitz WB. Electrical conversion of arrhythmias under diazepam
sedation. Conn Med 1969; 33:173-174.-44 Naney AP, Chaffee WG. Diazepam for cardioversion. JAMA 1971;
215:487. In the late 1970s and
1980s, midazolam replaced diazepam as first choice sedative for several procedures
basically due to its better amnesia properties.55 Al Khudhairi D, Whitwam JG, McCloy RF. Midazolam and diazepam for
gastroscopy. Anaesthesia 1982; 37:1002-1006.
6 Whitwam JG, Al Khudhairi D, McCloy RF. Comparison of midazolam and
diazepam in doses of comparable potency during gastroscopy. Br J Anaesth 1983;
55:773-777.
7 Brouillette DE, Leventhal R, Kumar S, Berman D, Kajani M, Yoo YK et al.
Midazolam versus diazepam for combined esophogastroduodenoscopy and colonoscopy. Dig
Dis Sci 1989; 34:1265-1271.
8 Krichbaum DW, Hamid I. Midazolam sedation and amnesia in elective
cardioversion. Clin Pharm 1988; 7:423.
9 Gupta A, Lennmarken C, Vegfors M, Tyden H. Anaesthesia for
cardioversion. A comparison between propofol, thiopentone and midazolam. Anaesthesia
1990; 45:872-875.
10 Gupta A, Vegfors M, Lennmarken C. Midazolam and cardioversion. Br J
Anaesth 1992; 69:422.
11 Dickinson ET, Cohen JE, Mechem CC. The effectiveness of midazolam as a
single pharmacologic agent to facilitate endotracheal intubation by paramedics.
Prehosp Emerg Care 1999; 3:191-193.
12 Schwander D, Sansano C. Cardiovascular changes during intubation with
midazolam as anaesthesia inducing agent. Arzneimittelforschung 1981;
31:2255-2260.
13 Boralessa H, Senior DF, Whitwam JG. Cardiovascular response to
intubation. A comparative study of thiopentone and midazolam. Anaesthesia 1983;
38:623-627.-1414 Sabbatani P, Mantovan R. Electrical cardioversion of atrial
fibrillation: Evaluation of sedation safety with midazolam by means of EtCO and IPI
algorithm analysis. Int J Cardiol 2013. It has repeatedly been
shown that physician-led sedation using the benzodiazepine diazepam is also safe and has
a positive impact on patient acceptability of the procedure.1515 Pugh PJ, Spurrell P, Kamalvand K, Sulke AN. Sedation by physician with
diazepam for DC cardioversion of atrial arrhythmias. Heart 2001;
86:572-573.,1616 Mitchell AR, Chalil S, Boodhoo L, Bordoli G, Patel N, Sulke N. Diazepam
or midazolam for external DC cardioversion (the DORM Study). Europace 2003;
5:391-395.
In several countries, benzodiazepines are still the main drug of choice for procedures instead of using newer, rapidly acting, anesthetics, largely driven by cost concerns.1616 Mitchell AR, Chalil S, Boodhoo L, Bordoli G, Patel N, Sulke N. Diazepam or midazolam for external DC cardioversion (the DORM Study). Europace 2003; 5:391-395. In the Santa Casa Hospital Complex (seven hospitals and eight ICUs), midazolam is the drug most used – and frequently solely used – for sedation in procedures like upper endoscopy, cardioversion or intubation.
The sedation time is reduced with midazolam compared with diazepam in several studies on
medical procedures but the differences are not clinically relevant.66 Whitwam JG, Al Khudhairi D, McCloy RF. Comparison of midazolam and
diazepam in doses of comparable potency during gastroscopy. Br J Anaesth 1983;
55:773-777.,1616 Mitchell AR, Chalil S, Boodhoo L, Bordoli G, Patel N, Sulke N. Diazepam
or midazolam for external DC cardioversion (the DORM Study). Europace 2003;
5:391-395.,1717 Staretz LR, Otomo-Corgel J, Lin JI. Effects of intravenous midazolam and
diazepam on patient response, percentage of oxygen saturation, and hemodynamic
factors during periodontal surgery. J Periodontol 2004;
75:1319-1326. The awakening time is
considerably longer for midazolam so that any time gained with induction of sedation is
lost in the longer recovery.1515 Pugh PJ, Spurrell P, Kamalvand K, Sulke AN. Sedation by physician with
diazepam for DC cardioversion of atrial arrhythmias. Heart 2001;
86:572-573.,1616 Mitchell AR, Chalil S, Boodhoo L, Bordoli G, Patel N, Sulke N. Diazepam
or midazolam for external DC cardioversion (the DORM Study). Europace 2003;
5:391-395.,1818 Zakko SF, Seifert HA, Gross JB. A comparison of midazolam and diazepam
for conscious sedation during colonoscopy in a prospective double-blind study.
Gastrointest Endosc 1999; 49:684-689.
19 Macken E, Gevers AM, Hendrickx A, Rutgeerts P. Midazolam versus diazepam
in lipid emulsion as conscious sedation for colonoscopy with or without reversal of
sedation with flumazenil. Gastrointest Endosc 1998; 47:57-61.-2020 Van Houten JS, Crane SA, Janardan SK, Wells K. A randomized,
prospective, double-blind comparison of midazolam (Versed) and emulsified diazepam
(Dizac) for opioid-based, conscious sedation in endoscopic procedures. Am J
Gastroenterol 1998; 93:170-174. However, most
patients that need urgent intubation in the ICU will need continuous sedation, mainly
due to respiratory insufficiency.
Studies examining the effects of midazolam reveal that they are similar to those of diazepam with few hemodynamic alterations.1616 Mitchell AR, Chalil S, Boodhoo L, Bordoli G, Patel N, Sulke N. Diazepam or midazolam for external DC cardioversion (the DORM Study). Europace 2003; 5:391-395.,1717 Staretz LR, Otomo-Corgel J, Lin JI. Effects of intravenous midazolam and diazepam on patient response, percentage of oxygen saturation, and hemodynamic factors during periodontal surgery. J Periodontol 2004; 75:1319-1326.,2121 Agelink MW, Majewski TB, Andrich J, Mueck-Weymann M. Short-term effects of intravenous benzodiazepines on autonomic neurocardiac regulation in humans: a comparison between midazolam, diazepam, and lorazepam. Crit Care Med 2002; 30:997-1006.,2222 Sanders LD, Davies-Evans J, Rosen M, Robinson JO. Comparison of diazepam with midazolam as i.v. sedation for outpatient gastroscopy. Br J Anaesth 1989; 63:726-731. Hypotension is observed with both diazepam and midazolam. This side effect can be of relevance when inducing sedation in a patient already hemodinamically unstable as several patients in need of urgent intubation.
There are no randomized trials comparing midazolam and diazepam for sedation in urgent oral-tracheal intubation. The finding of clinical equivalence between the two drugs in quality of sedation and adverse effects would allow institutions to choose between the agents on a drug cost basis. Eight years ago we performed a randomized study to compare both drugs during hospital financial crisis and a partial analysis of results was presented in an international congress.2323 Friedman G, Gehrke L, Oliveira RP, Becker M. Diazepam or Midazolam for Tracheal Intubation in the ICU? Intensive Care Med 2006; 32[supplement], S250. We are motivated to publish the results because the issue is up to date for several institutions in our country and others. Firstly, we hypothesized that diazepam and midazolam produce equal quality of sedation and, secondly, hemodynamic instability is equally significantly with both drugs. The main aim of this study was to compare the clinical effectiveness and after-effects of midazolam and diazepam in a single-blinded randomized design, during emergency intubation in the ICU. Also, we aimed to compare drug costs for adequate sedation during the procedure.
Methods
The local research ethical committee approved the study. The need for an informed consent was waived by the ethics committee as both drugs are commercially available and used by intensivists for the study procedure in the last thirty years. All patients admitted to the Central Intensive Care Unit of the Santa Casa Hospital Complex in Porto Alegre, over the age of 18 years, undergoing the first urgent intubation during ICU stay between May 2005 and October 2005 were eligible for the study. Patients were excluded if they had allergy to either drug, or if they were already under sedation. Immediately after decision to intubate, once all inclusion and exclusion criteria were met, patients were randomized in a single-blinded manner (opaque sealed envelopes) to either diazepam or midazolam for intravenous sedation during the procedure. Patients or families were not told which type of sedation they received but operators were unblinded.
All intubations were coordinated by a senior intensivist of the staff. Pre-intubation protocol followed our standard procedures for preparation (i.e. positioning, oxymeter, monitor) and preoxygenation before medication. The attending doctor administered the sedative according to a titration protocol. Diazepam was given as a 5 mg intravenous bolus followed by aliquots of 5 mg each minute. Midazolam was given as an intravenous bolus of 5 mg with further aliquots of 2.5 mg each minute. The use of an opioid (morphine or fentanyl) or neuromuscular blockers was allowed at discretion of the attending doctor. ECG, oxygen saturation, respiratory rate, and blood pressure monitoring were performed continuously throughout the procedure. Adequate sedation was considered whenever a Ramsay sedation scale 5-6 was reached.
Sedation time was recorded as the time from first injection to the time of adequate sedation. Oral-tracheal intubation was performed according to the standard ICU procedure. Each patient was observed during 60 min since first injection, every 15 minutes and thereafter continuously received sedation and analgesia to facilitate mechanical ventilation. During the observation period, we evaluated required doses of each drug, time to adequate sedation and duration of sedation. The following demographic variables were collected for all patients: age, gender, admission diagnosis, Acute Physiology and Chronic Health Evaluation II severity score (Apache II).2424 Knaus WA, Draper EA, Wagner DP, Zimmerman JE. Apache II: a severity of disease classification system. Crit Care Med 1985; 13:818-829.
Statistics
Data are presented as mean±standard deviation or median (25-75 percentiles) according to the statistical test used. Comparisons of non-parametric data were by Mann-Whitney U tests. Parametric data were compared with unpaired Student’s t tests. Cardiovascular and oxygenation parameters at each time were analyzed with a two-way repeated measures analysis of variance with post hoc Dunnett’s test (within groups) and single degree of freedom tests (between groups) when significance was detected. Nominal data were analyzed by Chi-square or Fisher’s exact test, as appropriate. P <0.05 was considered significant. Calculation of sample size indicated 17 patients in each group with a power of 0.8 and alpha 0.05, based on a pilot study after inclusion of 5 patients in each group and using a 30% difference on time for adequate sedation as outcome.
Results
Between May 2005 and October 2005, 76 patients were intubated in the Central Intensive Care Unit. Twenty five patients were excluded from the study because they were under sedatives prior to intubation. Twenty patients were excluded because the assistant intensivist decided to use another sedative (e.g. propofol) or the intubation was considered urgent and no randomization was performed. Thirty four patients were randomized, but one patient in the diazepam group was excluded from the analysis because all data were lost. Patients’ characteristics are shown in Table 1. Both groups were similar in terms of illness severity and demographic data.
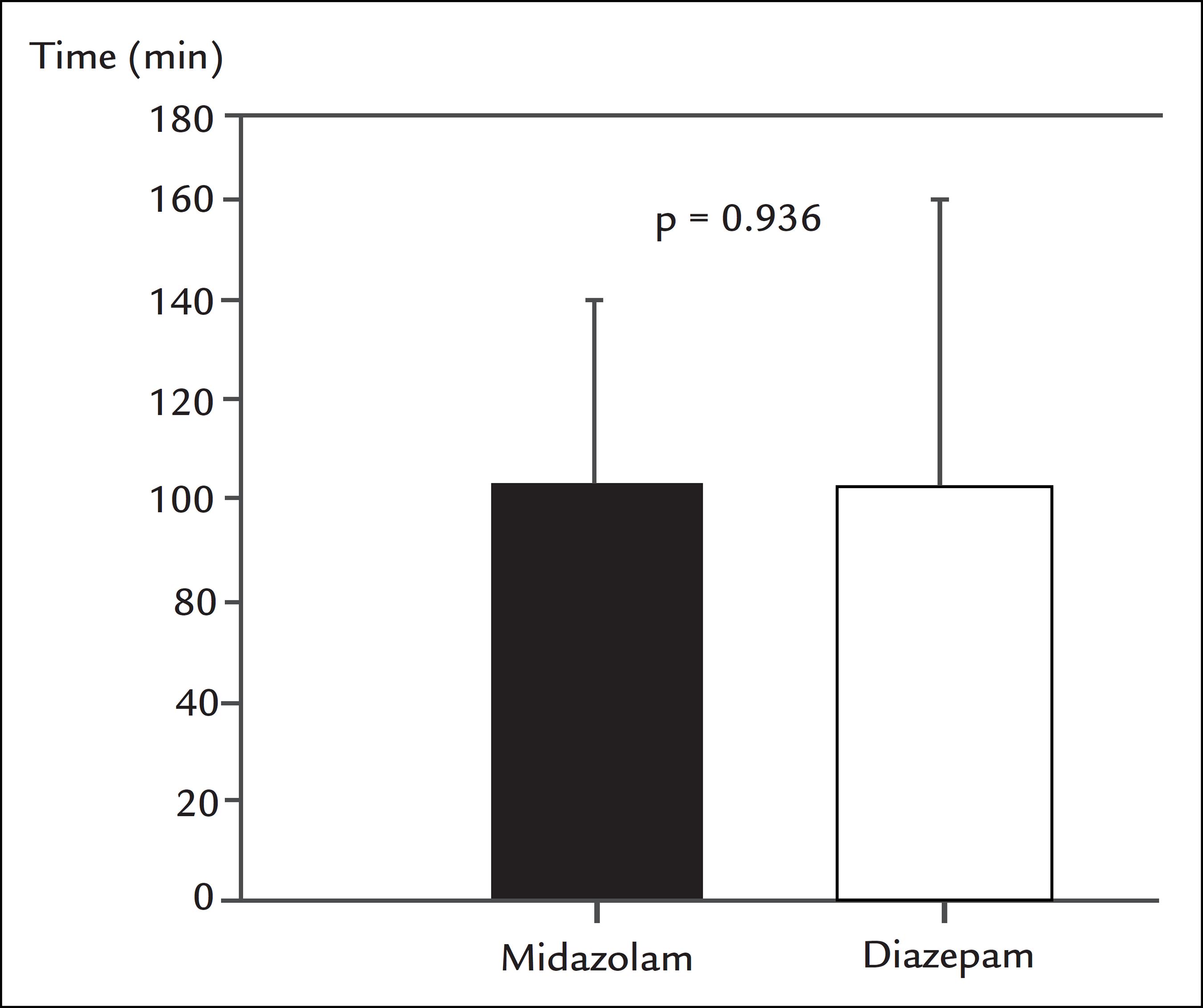
Time for adequate sedation (Figure 1) was shorter but duration of sedation was similar for diazepam in comparison to midazolam (Figure 2). Total drug dose to reach adequate sedation after intravenous diazepam or midazolam was not different (10.0 [10.0-12.5] mg vs. 15.0 [10.0-17.5] mg, p = 0.248). There were no differences between study drugs during time for cardiorespiratory parameters or sedation intensity (Table 2). Arterial pressure and Ramsay scale reduced significantly after 15 minutes for both drugs. The proportion of patients that experienced hypotension (Systolic pressure < 90 mmHg) was similar for midazolam and diazepam (10 patients vs. 10 patients). Four patients received a bolus of fentanyl in the midazolam and diazepam groups (130 ± 26 µg vs. 125 ± 19 µg, p = 0.76). One patient received a 5 mg bolus of morphine in the midazolam group. None of the patients was intubated under paralysis.
Time for adequate sedation (Ramsay sedation scale 5-6) was shorter after intravenous diazepam (n=16) in comparison to midazolam (n=17).
Duration of sedation (min) until Ramsay scale <5 after intravenous midazolam (n=17) or diazepam (n=16) was similar.
Time changes in and cardiorespiratory parameters and Ramsey scale after intravenous midazolam (n=17) or diazepam (n=16)
Single use ampoules were used and excess drug was discarded between cases. The current (January-2014) cost of sedation (syringes and ampoules) with diazepam, 1.40 [1.40-1.85] reais, was significantly lower than with midazolam, 13.90 [9.40-16.25] reais, p <0.001.
Senior intensivists were not required in any of the intubations.
Discussion
This study showed that both midazolam and diazepam were safe and well tolerated for physician-led sedation during urgent oral-tracheal intubation. At the doses used, they were equally effective and without major adverse events following the procedure.
Important differences between the clinical effects of the studied drugs when used in
this manner were identified. Surprisingly, the sedation time was significantly reduced
with diazepam compared with midazolam. In comparative studies with diazepam in several
procedures, midazolam proved more effective at inducing rapid sedation.1616 Mitchell AR, Chalil S, Boodhoo L, Bordoli G, Patel N, Sulke N. Diazepam
or midazolam for external DC cardioversion (the DORM Study). Europace 2003;
5:391-395.,1818 Zakko SF, Seifert HA, Gross JB. A comparison of midazolam and diazepam
for conscious sedation during colonoscopy in a prospective double-blind study.
Gastrointest Endosc 1999; 49:684-689.
19 Macken E, Gevers AM, Hendrickx A, Rutgeerts P. Midazolam versus diazepam
in lipid emulsion as conscious sedation for colonoscopy with or without reversal of
sedation with flumazenil. Gastrointest Endosc 1998; 47:57-61.-2020 Van Houten JS, Crane SA, Janardan SK, Wells K. A randomized,
prospective, double-blind comparison of midazolam (Versed) and emulsified diazepam
(Dizac) for opioid-based, conscious sedation in endoscopic procedures. Am J
Gastroenterol 1998; 93:170-174. Midazolam is known to
be rapidly absorbed and the onset of action is, therefore, faster than that of diazepam
and its effects are expected to occur sooner than those of diazepam.
In addition, the dose of both drugs to reach adequate sedation was similar. This finding is in contrast to several studies that have shown than midazolam is 2-3 times more potent than diazepam.1616 Mitchell AR, Chalil S, Boodhoo L, Bordoli G, Patel N, Sulke N. Diazepam or midazolam for external DC cardioversion (the DORM Study). Europace 2003; 5:391-395.,1717 Staretz LR, Otomo-Corgel J, Lin JI. Effects of intravenous midazolam and diazepam on patient response, percentage of oxygen saturation, and hemodynamic factors during periodontal surgery. J Periodontol 2004; 75:1319-1326. We speculated that although this finding looks contradictory, a wide individual variation in dose-effect response was seen, as shown by the range of total dosages required in this study. These wide variations in response are typical of benzodiazepines and may be partly explained by high plasma protein binding.2525 Henthorn TK, Krejcie TC, Avram MJ. Early drug distribution: a generally neglected aspect of pharmacokinetics of particular relevance to intravenously administered anesthetic agents. Clin Pharmacol Ther 2008; 84:18-22.,2626 Olkkola KT, Ahonen J. Midazolam and other benzodiazepines. Handb Exp Pharmacol 2008; 182:335-360. Obese patients have an increased volume of distribution due to enhanced distribution in peripheral adipose tissues and interactions with other drugs that are metabolized through the cytochrome p450 system can influence the clinical response.2727 Oldenhof H, de Jong M, Steenhoek A, Janknegt R. Clinical pharmacokinetics of midazolam in intensive care patients, a wide interpatient variability? Clin Pharmacol Ther 1988; 43:263-269. Benzodiazepines have synergistic interactions with other drugs like opioids that were simultaneously used in most patients. Pharmacokinetics of almost all drugs, including sedatives, are not well known in critically ill patients.2828 Roberts DJ, Haroon B, Hall RI. Sedation for critically ill or injured adults in the intensive care unit: a shifting paradigm. Drugs 2012; 72:1881-1916.,2929 Escobar L, Gai MN, Regueira T, Andresen M. Pharmacokinetic considerations in critically ill patients. Rev Med Chil 2012; 140:780-788.
The reduction in blood pressure and the incidence of hypotension observed with midazolam and diazepam (60% of patients) may have been related to the high doses used to achieve rapid sedation in already sick patients prone to hemodynamic instability. Fifteen episodes of hypotension in this study occurred within the first 15 minutes. It has been shown that the use of both diazepam and midazolam is associated with decreased systolic blood pressure.3030 Raza SM, Masters RW, Zsigmond EK. Comparison of the hemodynamic effects of midazolam and diazepam in patients with coronary occlusion. Int J Clin Pharmacol Ther Toxicol 1989; 27:1-6. Midazolam is particularly associated with reduction in both systemic vascular resistance and diastolic pressure.3030 Raza SM, Masters RW, Zsigmond EK. Comparison of the hemodynamic effects of midazolam and diazepam in patients with coronary occlusion. Int J Clin Pharmacol Ther Toxicol 1989; 27:1-6.
The lower cost with diazepam is an important finding. Although both drugs have generic presentations with lowering costs in the last decade, diazepam costs were much lower both because one milligram of diazepam is cheaper than one milligram of midazolam and the concentration used for the same sedative effect was smaller. Although cost evaluation was not precise because we did not include expenses with diluents, for instance, drug cost itself accounts for the greater part of it. The cost of one syringe was 0.4 real and for most cases a single one was needed.
The study has several limitations. The study was single-blinded and operator observations may have been influenced by individual experience and preference with each form of sedation. Due to the different titration properties and appearance of the two drugs, blinding the drug to the operator was not ideal. No adjustments were made in this study for body weight or concomitant drug use. We used the end-point of Ramsay scale 5-6 to indicate an adequate level of sedation. Despite the scale of Ramsay being mostly used these days, there is good correlation with other scales, particularly the Richmond Agitation-Sedation scale, and our end point was deep sedation which has excellent equivalence in most scales.3131 Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 2003; 289:2983-2991. In addition, both groups included patients with somewhat low Glasgow coma scale or previous strokes that could interfered the sedation evaluation. The study is 8 years old and medical practices may have changed. For instance, the use of rapid sequence intubation as a standard protocol is not yet well incorporated by most physicians, both in our ICU and emergency room. However, the use of midazolam is still the most current practice for hundreds of procedures performed in more than 110 ICU adult beds in our Hospital Complex.
Physician-led intubation using intravenous diazepam and midazolam is highly effective and well tolerated, with only minor effects. Sedation with diazepam is associated to a quicker sedation time than midazolam and to lower costs.
References
-
1Kahler RL, Burrow GN, Felig P. Diazepam-induced amnesia for cardioversion. JAMA 1967; 200:997-998.
-
2Nutter DO, Massumi RA. Diazepam in cardioversion. N Engl J Med 1965; 273(12):650-651.
-
3Lebowitz WB. Electrical conversion of arrhythmias under diazepam sedation. Conn Med 1969; 33:173-174.
-
4Naney AP, Chaffee WG. Diazepam for cardioversion. JAMA 1971; 215:487.
-
5Al Khudhairi D, Whitwam JG, McCloy RF. Midazolam and diazepam for gastroscopy. Anaesthesia 1982; 37:1002-1006.
-
6Whitwam JG, Al Khudhairi D, McCloy RF. Comparison of midazolam and diazepam in doses of comparable potency during gastroscopy. Br J Anaesth 1983; 55:773-777.
-
7Brouillette DE, Leventhal R, Kumar S, Berman D, Kajani M, Yoo YK et al. Midazolam versus diazepam for combined esophogastroduodenoscopy and colonoscopy. Dig Dis Sci 1989; 34:1265-1271.
-
8Krichbaum DW, Hamid I. Midazolam sedation and amnesia in elective cardioversion. Clin Pharm 1988; 7:423.
-
9Gupta A, Lennmarken C, Vegfors M, Tyden H. Anaesthesia for cardioversion. A comparison between propofol, thiopentone and midazolam. Anaesthesia 1990; 45:872-875.
-
10Gupta A, Vegfors M, Lennmarken C. Midazolam and cardioversion. Br J Anaesth 1992; 69:422.
-
11Dickinson ET, Cohen JE, Mechem CC. The effectiveness of midazolam as a single pharmacologic agent to facilitate endotracheal intubation by paramedics. Prehosp Emerg Care 1999; 3:191-193.
-
12Schwander D, Sansano C. Cardiovascular changes during intubation with midazolam as anaesthesia inducing agent. Arzneimittelforschung 1981; 31:2255-2260.
-
13Boralessa H, Senior DF, Whitwam JG. Cardiovascular response to intubation. A comparative study of thiopentone and midazolam. Anaesthesia 1983; 38:623-627.
-
14Sabbatani P, Mantovan R. Electrical cardioversion of atrial fibrillation: Evaluation of sedation safety with midazolam by means of EtCO and IPI algorithm analysis. Int J Cardiol 2013.
-
15Pugh PJ, Spurrell P, Kamalvand K, Sulke AN. Sedation by physician with diazepam for DC cardioversion of atrial arrhythmias. Heart 2001; 86:572-573.
-
16Mitchell AR, Chalil S, Boodhoo L, Bordoli G, Patel N, Sulke N. Diazepam or midazolam for external DC cardioversion (the DORM Study). Europace 2003; 5:391-395.
-
17Staretz LR, Otomo-Corgel J, Lin JI. Effects of intravenous midazolam and diazepam on patient response, percentage of oxygen saturation, and hemodynamic factors during periodontal surgery. J Periodontol 2004; 75:1319-1326.
-
18Zakko SF, Seifert HA, Gross JB. A comparison of midazolam and diazepam for conscious sedation during colonoscopy in a prospective double-blind study. Gastrointest Endosc 1999; 49:684-689.
-
19Macken E, Gevers AM, Hendrickx A, Rutgeerts P. Midazolam versus diazepam in lipid emulsion as conscious sedation for colonoscopy with or without reversal of sedation with flumazenil. Gastrointest Endosc 1998; 47:57-61.
-
20Van Houten JS, Crane SA, Janardan SK, Wells K. A randomized, prospective, double-blind comparison of midazolam (Versed) and emulsified diazepam (Dizac) for opioid-based, conscious sedation in endoscopic procedures. Am J Gastroenterol 1998; 93:170-174.
-
21Agelink MW, Majewski TB, Andrich J, Mueck-Weymann M. Short-term effects of intravenous benzodiazepines on autonomic neurocardiac regulation in humans: a comparison between midazolam, diazepam, and lorazepam. Crit Care Med 2002; 30:997-1006.
-
22Sanders LD, Davies-Evans J, Rosen M, Robinson JO. Comparison of diazepam with midazolam as i.v. sedation for outpatient gastroscopy. Br J Anaesth 1989; 63:726-731.
-
23Friedman G, Gehrke L, Oliveira RP, Becker M. Diazepam or Midazolam for Tracheal Intubation in the ICU? Intensive Care Med 2006; 32[supplement], S250.
-
24Knaus WA, Draper EA, Wagner DP, Zimmerman JE. Apache II: a severity of disease classification system. Crit Care Med 1985; 13:818-829.
-
25Henthorn TK, Krejcie TC, Avram MJ. Early drug distribution: a generally neglected aspect of pharmacokinetics of particular relevance to intravenously administered anesthetic agents. Clin Pharmacol Ther 2008; 84:18-22.
-
26Olkkola KT, Ahonen J. Midazolam and other benzodiazepines. Handb Exp Pharmacol 2008; 182:335-360.
-
27Oldenhof H, de Jong M, Steenhoek A, Janknegt R. Clinical pharmacokinetics of midazolam in intensive care patients, a wide interpatient variability? Clin Pharmacol Ther 1988; 43:263-269.
-
28Roberts DJ, Haroon B, Hall RI. Sedation for critically ill or injured adults in the intensive care unit: a shifting paradigm. Drugs 2012; 72:1881-1916.
-
29Escobar L, Gai MN, Regueira T, Andresen M. Pharmacokinetic considerations in critically ill patients. Rev Med Chil 2012; 140:780-788.
-
30Raza SM, Masters RW, Zsigmond EK. Comparison of the hemodynamic effects of midazolam and diazepam in patients with coronary occlusion. Int J Clin Pharmacol Ther Toxicol 1989; 27:1-6.
-
31Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 2003; 289:2983-2991.
Publication Dates
-
Publication in this collection
Feb 2015
History
-
Received
06 Apr 2014 -
Accepted
03 June 2014