Abstracts
PURPOSE: To present an alternative technique for reconstruction of musculocutaneous damages in the face transferring innervated subsegments(subunits) of the latissimus dorsi flap for replacement of various facial mimetic muscles. METHODS: One clinical case of trauma with skin and mimetic muscles damage is described as an example of the technique. The treatment was performed with microsurgical transfer of latissimus dorsi muscle subunits. Each subunit present shape and dimensions of the respective mimetic muscles replaced. The origin, insertions and force vectors for the mimicmuscle lost were considered. Each subsegment has its own arterial and venous supply with a motor nerve component for the muscular unit. RESULTS: Pre and one year postoperative photos registration of static and dynamic mimic aspects, as well as digital electromyography digital data of the patients were compared. The transplanted muscular units presented myoeletric activity, fulfilling both the functional and cosmetic aspect. CONCLUSION: This technique seems to be a promising way to deal with the complex musculocutaneous losses of the face as well as facial palsy.
Facial Paralysis; Reconstruction; Facial Muscles; Microsurgery
OBJETIVO: Apresentar uma alternativa técnica para reconstrução de perdas músculo-cutâneas na face com a transferência de sub-segmentos(sub-unidades) inervados do músculo grande dorsal para a substituição dos diversos músculos da mímica facial. MÉTODOS: É descrito um caso de trauma com perda de pele e músculo da mímica. Foi corrigido com a transferência microcirúrgica de uma sub-unidade de músculo grande dorsal que apresenta, forma, tamanho e peso similares aos dos músculos da mímica. Respeitou-se as origens e inserções e vetores de ação para a mímica desejada. Cada um dos sub-segmentos têm artéria e veia que irrigam a unidade muscular e também um nervo com componente motor. RESULTADOS: O paciente foi avaliado comparando-se o pré e pós-operatório de um ano com foto e vídeo com mímica em repouso e dinâmica e eletromiografia (documentada em vídeo digital). Observou-se atividade mio-elétrica dos músculos transplantados. Verificou-se que a técnica foi eficaz do ponto de vista funcional e estético. CONCLUSÃO: Esta técnica parece ser uma maneira eficaz para tratar as deformidades pós-perdas complexas de pele e músculos da face e no tratamento da paralisia facial.
Paralisia Facial; Reconstrução; Músculos Faciais; Microcirurgia
PRELIMINARY REPORT
Muscular subunits transplantation for facial reanimation1 1 . Study performed at the Division of Reconstructive Microsurgery of the Souza Aguiar City Hospital, Rio de Janeiro, Brazil, and at the Division of Plastic Surgery of the Federal University of São Paulo, São Paulo, Brazil.
Transplantes de sub-unidades musculares na reanimação facial
André Salo Buslik HazanI; Fábio Xerfan NahasII; Rodrigo Tiago FariaIII; Ramil SinderIV; Lydia Masako FerreiraV
IChairman of Reconstructive Microsurgery of the Souza Aguiar City Hospital, Rio de Janeiro, Brazil
IIAssociate Professor of the Plastic Surgery Division of Federal University of São Paulo, São Paulo, Brazil
IIIFellow of the Reconstructive Microsurgery Division of the Souza Aguiar City Hospital, Rio de Janeiro, Brazil
IVFull Professor of the Plastic Surgery Division of the Fluminense Federal University, Rio de Janeiro, Brazil
VFull Professor of the Plastic Surgery Division of the Federal University of São Paulo, São Paulo, Brazil
Correspondence Correspondence: André Hazan Plastic Surgery Division of Federal University of São Paulo Rua Napoleão de Barros, 715/4º andar 04024-0900 São Paulo SP Brazil Phone : (55 11)5576-4118 andrehazan@hotmail.com
ABSTRACT
PURPOSE: To present an alternative technique for reconstruction of musculocutaneous damages in the face transferring innervated subsegments(subunits) of the latissimus dorsi flap for replacement of various facial mimetic muscles.
METHODS: One clinical case of trauma with skin and mimetic muscles damage is described as an example of the technique. The treatment was performed with microsurgical transfer of latissimus dorsi muscle subunits. Each subunit present shape and dimensions of the respective mimetic muscles replaced. The origin, insertions and force vectors for the mimicmuscle lost were considered. Each subsegment has its own arterial and venous supply with a motor nerve component for the muscular unit.
RESULTS: Pre and one year postoperative photos registration of static and dynamic mimic aspects, as well as digital electromyography digital data of the patients were compared. The transplanted muscular units presented myoeletric activity, fulfilling both the functional and cosmetic aspect.
CONCLUSION: This technique seems to be a promising way to deal with the complex musculocutaneous losses of the face as well as facial palsy.
Key words: Facial Paralysis. Reconstruction. Facial Muscles. Microsurgery.
RESUMO
OBJETIVO: Apresentar uma alternativa técnica para reconstrução de perdas músculo-cutâneas na face com a transferência de sub-segmentos(sub-unidades) inervados do músculo grande dorsal para a substituição dos diversos músculos da mímica facial.
MÉTODOS: É descrito um caso de trauma com perda de pele e músculo da mímica. Foi corrigido com a transferência microcirúrgica de uma sub-unidade de músculo grande dorsal que apresenta, forma, tamanho e peso similares aos dos músculos da mímica. Respeitou-se as origens e inserções e vetores de ação para a mímica desejada. Cada um dos sub-segmentos têm artéria e veia que irrigam a unidade muscular e também um nervo com componente motor.
RESULTADOS: O paciente foi avaliado comparando-se o pré e pós-operatório de um ano com foto e vídeo com mímica em repouso e dinâmica e eletromiografia (documentada em vídeo digital). Observou-se atividade mio-elétrica dos músculos transplantados. Verificou-se que a técnica foi eficaz do ponto de vista funcional e estético.
CONCLUSÃO: Esta técnica parece ser uma maneira eficaz para tratar as deformidades pós-perdas complexas de pele e músculos da face e no tratamento da paralisia facial.
Descritores: Paralisia Facial. Reconstrução. Músculos Faciais. Microcirurgia.
Introduction
The correction of defects after mimetic muscles damage, associated or not to skin loss, has been a great challenge for reconstructive surgeons. Several flaps were used for the treatment of this deformity, such as local flaps, musculocutaneous flaps1, free innervated fasciocutaneous flaps3 and recently the ones of perforator flaps12 which allows reduction of the thickness of the flap. However, perforator flaps offer cutaneous cover only. The use of muscular flaps4,5,6,7,8,9,10,11,15,16 has been previously performed and showed restrictions because of the large volume of muscle transferred and the vector in a single direction. The greatest challenges for reconstruction of this area are the complex defects involving muscle and skin. The currently available techniques offer the muscular segments as a tool for restoring the labial comissure mobilization. However, these techniques do not allow the replacement of muscles with similar size and thickness of the damaged multiple mimetic muscles of the face with different force vectors. The purpose of this study is to present an alternative reconstruction technique for musculocutaneous losses of the face by transferring innervated subunits of latissimus dorsi muscle to replace the various facial mimetic muscles.
Case description
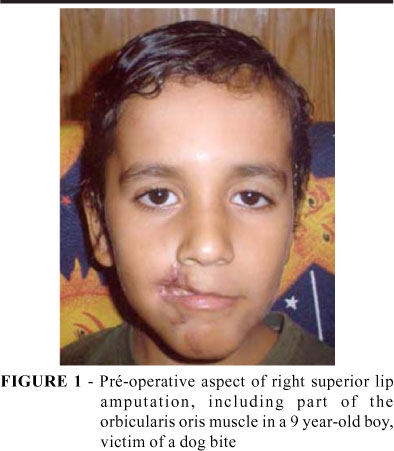
Case: Male patient, 9 years old, victim of dog bite.
The patient presented an amputation of the right region of the upper lip, including the corresponding portion of the orbicularis oris muscle (Figures 1 to 6). The treatment proposed was an autogenous neurovascular supplied flap of a subunit of the latissimus dorsi muscle with overlying cutaneous portion, associated to neurovascular supplied by perforators (Figure 7). The distal attachments of the adjacent muscles were repositioned on the muscular flap (Figure 8). The teeth, formerly exposed, did not show after reconstruction (Figures 1 to 4).
Surgical procedure (Technique)
The patient is positioned in lateral decubitus, under general anesthesia. The lateral border of latissimus dorsi muscle is reference for the skin incision. The perforators vessels are identified. These vessels have at least 0.4 a 0.6mm in diameter and the vessel that supplies the overlying skin is individualized. These vessels are located between 4-6cm from imaginary line that passes on the inferior angle border of the scapula and about 2-3cm posterior to the lateral border of the latissimus dorsi muscle12. Dissection proceeds into the muscle, sectioning the epimysium and the perimysium, individualizing the lateral segmental bundle14 or the inferior one12. Then, the vascular14 and nervous subsegmental bundles penetrating the corresponding muscular groups are observed. The neurovascular subsegmental bundles and the muscular subunits are isolated by dissection.
The bleeding in the muscular portion is checked. After bleeding is observed the muscular subunits are transferred with the subsegmental branches that originate from the lateral segmentar vessel, a branch of the thoracodorsal that are last rami of the subscapular vessels pedicle which it is used for the microsurgical anastomosis. The only lateral segmental nerve transferred is the one correspondent to the muscular segmental flap to be transferred. The medial (or superior) segmental branch of the nerve is preserved. The facial or temporal vessels can be used as receptors. The buccal and the mandibular marginal branches of the facial nerve can be the receptors of the lateral segmental ramus of the thoracodorsal nerve. Nylon 10-0 for epi-perineural end to end synthesis with interrupted sutures was used in this case. Muscle synthesis was performed with absorbable sutures, inserting them between the remaining parts of the damaged muscles. When necessary, the muscles can be attached to the periosteum and to other muscles. The origin and distal attachment vectors of the transferred muscles were also considered in order to simulate the vectors of the injured muscles.
Functional evaluation
After one year of surgery, the videos and digital photos with static and dynamic mimic and EMG, registered before and after surgical reconstruction were compared. After ten months all the muscles were tested with EMG. The EMG study was performed with a Neuropack II model® and concentric needle NM320 T (Nihon-Khoden®, Japan), that captures stimuli of the punctured muscle. The concentric needle has the advantage of reducing the possible contamination of stimuli of other muscles. Myoeletric activity was demonstrated when the patient was asked to perform contractions corresponding to the action of the mimetic facial muscle injured by trauma.
Discussion
The main goal of damaged mimic muscles reconstruction is to preserve muscular function, adequate mouth opening and an acceptable aesthetic appearance. All currently available reconstruction techniques have limitations such as microstomy, lack of mobility, large muscular volume and they do not permit a reconstruction of multiple muscles of the face. Zhao et al.14, on El-Maasarany et al.13, published a study on the anatomy of the muscular segments of the latissumus dorsi muscle for reconstruction of facial paralysis. The flaps described in the present study are multiple subsegmental muscles with specific subsegmental vessels and nerves (Figure 11).
In this study, subunits of independent muscles were created (Figures 8 and 11). They are supplied by a subsegmental vessels pedicle connected to a lateral or inferior segmental vessel, which is a branch of the thoracodorsal vessel. The artery, two veins and a nerve run together through a connective tissue, supplying many subsegments as studied in cadavers, previously to the use of this technique in patients (Figures 10 and 11).
The electromyographic study (EMG) showed myoelectric activity of the transplanted muscles when resting and contracting. The data were similar to the ones obtained from the normal opposite muscles. The advantage of these flaps for reconstruction of musculocutaneous damage of the face is that they are able to simulate the size and thickness of the muscles of the face, positioned in different vectors. This type of flap will allow us, in the near future, to reconstruct the whole side of a paralyzed face, in case of sequel of facial reanimation. Or even the whole face as alternative for homologous transplant in patients with severe functional avulsions and burns of the face as well as following tumor resections. To sum up, the results of this technique seem to be promising since oral continence, full function with myoeletric activity signs on EMG were observed.
Acknowledgments
Deolindo Couto's Institute of Neurology of Universidade Federal do Rio de Janeiro (UFRJ) and Dr. Glória Penque (MD), neurologist and neurophysiologist for the availability and seriousness while performing EMGs (electromyographies). Forensic Medicine Afrânio Peixoto Institute of Rio de Janeiro to permit the cadaver dissections.
Received: October 05, 2005
Review: November 09, 2005
Accepted: December 08, 2005
Conflict of interest: none
Financial source: none
How to cite this article: Hazan ASB, Nahas FX, Faria RT, Sinder R, Ferreira LM. Muscular subunits transplantation for facial reanimation. Acta Cir Bras. [serial on the Internet] 2006 Mar-Apr;21(2). Available from URL: http://www.scielo.br/acb
- 1. Rashid M, Hanif MS, ILLAHI I, Aslam R, Hameed S, Masood T. Reconstruction of lip defects with the Kaparandzic technique. J Coll Physicians Surg Pak. 2003; 13(4):219-22.
- 2. Wechselberger G, Gurunluoglu R, Bauer T, Piza-Katzer H, Schoeller T. Functional lower lip reconstruction with bilateral cheek advancement flaps: revisitation of Webster method with a minor modification in the technique. Aesth Plast Surg. 2002; 26(6): 423-8.
- 3. Ozdemir R, Ortak T, Kocer U, Celebioglu S, Sensoz O, Tifikcioglu YO. Total lower lip reconstruction using sensate composite radial forearm flap. J Craniofac Surg. 2003; 14(3): 393-405.
- 4. Harii K. Microneurovascular free muscle transplantation for reanimation of facial paralysis. Clin Plast Surg. 1979; 6 (3): 361-75.
- 5. Harii k, Asato H, Yoshimura K, Sugawara Y, Nakatsuka T, Ueda K. One-stage transfer of the latissimus dorsi muscle for reanimation of a paralyzed face: a new alternative. Plast Reconstr Surg 1998; 102(4):941-51.
- 6. Dellon AL, Mackinnon SE. Segmentally innervated latissimus dorsi muscle. Microsurgical transfer for facial reanimation. J Reconstr Microsurg. 1985; 2(1): 7-12.
- 7. Mackinnon SE, Dellon AL. Technical considerations of the latissimus dorsi flap: a segmentally muscle transfer for facial reanimation. Microsurgery. 1998; 9 (1):36-45.
- 8. Sassoon EM, Poole MD. Rushworth G. Reanimation for facial palsy using gracilis muscle grafts. Br J Plast Surg. 1991; 44(3)195-200.
- 9. Kumar PA. Cross-face reanimation of the paralyzed face, with a single stage microneurovascular gracilis transfer without nerve graft: a preliminary report. Br J Plast Surg. 1995; 48(7):519-20.
- 10. Jones BM. Cross-face reanimation of the paralyzed face with a single stage microneurovascular gracilis transfer without nerve graft. Br J Plast Surg. 1995; 48(7):519-20.
- 11. Lifchez SD, Matloub HS, Gosain AK. Cortical adaptation to restoration of smiling after free muscle transfer innervated by the nerve to the masseter. Plast Reconstr Surg. 2005; 115(6):1472-9.
- 12. Angrigiani C, Grili D, Siebert J. Latissimus dorsi musculocutaneous flap without muscle. Plast Reconstr Surg. 1995;96(7):1608-14.
- 13. SH El-Maasarany, E Sharaf, F Moustafa, A Borhan, A Abdel-fattah, A Hamza. Anatomical basis of latissimus dorsi myocutaneous flap: clinical applications. Surg Radiol Anat. 1989; 11:197-203.
- 14. Zhao L, Miao H, Wang W and Zhang D. The anatomy of the segmental latissimus dorsi flap for reconstruction of facial paralysis. Surg Radiol Anat(1993); 15:239-43.
- 15. Maral T, Ozcan G. Functional reconstruction of the lateral face after ablative tumor resection: use free muscle and musculocutaneous flaps. Head Neck. 2001; 23(10):836-43.
- 16. Safak T, Akyurek M. Primary one-stage reconstruction of cheek defect after a shotgun blast to the face: use of the latissimus dorsi musculocutaneous free flap for soft-tissue repair and facial reanimation. Ann Plast Surg. 2001; 47 (4):438-41.
Publication Dates
-
Publication in this collection
21 Mar 2006 -
Date of issue
Apr 2006
History
-
Accepted
08 Dec 2005 -
Reviewed
09 Nov 2005 -
Received
05 Oct 2005