ABSTRACT
BACKGROUND AND OBJECTIVES:
The objective of this study was to evaluate the effect of neural mobilization technique on individuals with chronic low back pain, as well as analyze possible changes in pain, motor behavior and on cytokine quantification before and after treatment.
METHODS:
Sixteen individuals with mean age of 30.45±10.32 years old were evaluated. The technique consisted of a total of 10 interventions, with a total duration of 10 minutes, divided into four series of 2 minutes each, with a 30-second interval between each series. The following outcomes were evaluated: pain intensity using the visual analog scale; mobility of the lumbar spine with the third finger to the ground test and hip goniometry; concentration of cytokines in serum with the multiplex technique; and quality of life with the Oswestry Disability Index, the Roland-Morris Disability Questionnaire and the World Health Organization Quality of Life Questionnaire-bref.
RESULTS:
Results showed a reduction in pain intensity of approximately 70% between the assessments (p<0.001). Improvements in lumbar mobility of approximately 25.5% on the third finger to the ground test (p<0.04) and improvement in the hip joint angles (p<0.04) were also observed. A difference in cytokine concentrations, both pro-inflammatory (p<0.009) and anti-inflammatory (p<0.03), was also observed between the assessments.
CONCLUSION:
The technique was able to reduce pain intensity and consequently increase the mobility of the volunteers. Additionally, a difference in cytokine concentration at the end of the treatment and an improvement in the individuals quality of life were observed.
Keywords:
Low back pain; Pain; Quality of life
RESUMO
JUSTIFICATIVA E OBJETIVOS:
O objetivo deste estudo foi avaliar o efeito da técnica de mobilização neural em indivíduos com lombalgia crônica, assim como possíveis alterações na dor, no comportamento motor e na quantificação de citocinas antes e após o tratamento.
MÉTODOS:
Foram avaliados 16 indivíduos com idade média de 30,45±10,32 anos. A técnica consistiu em um total de 10 intervenções, com duração total de 10 minutos, divididas em quatro séries de 2 minutos cada, com intervalo de 30 segundos entre cada série. Os desfechos a seguir foram avaliados: intensidade da dor utilizando a escala analógica visual; mobilidade da coluna lombar com o terceiro dedo ao solo e goniometria do quadril; concentração de citocinas no soro com a técnica multiplex; e qualidade de vida com o Oswestry Disability Index, Roland-Morris Disability Questionnaire and the World Health Organization Quality of Life Questionnaire-bref.
RESULTADOS:
Os presentes resultados demonstraram uma redução na intensidade da dor de aproximadamente 70% entre as avaliações (p<0,001). Foram observadas melhoras na mobilidade lombar de aproximadamente 25,5% no teste do terceiro dedo ao solo (p<0,04) e nos ângulos da articulação do quadril (p<0,04). Também foi observada entre as avaliações diferença nas concentrações de citocinas, tanto pró-inflamatórias (p<0,009) quanto anti-inflamatórias (p<0,03).
CONCLUSÃO:
A técnica foi capaz de reduzir a intensidade da dor e consequentemente aumentar a mobilidade dos voluntários. Além disso, foi observada uma diferença na concentração de citocinas no final do tratamento e uma melhoria na qualidade de vida dos indivíduos.
Descritores:
Dor; Dor lombar; Qualidade de vida
INTRODUCTION
The term low back pain is characterized mainly by pain in the lumbar spine region, a condition that affects individuals of both sexes and reduces their ability to perform activities in their daily lives, which results in a substantial economic cost to society(11 Briganó JU, Macedo CSG. Análise da mobilidade lombar e influência da terapia manual e cinesioterapia na lombalgia. Semina: Ciências Biológicas e da Saúde. 2005;26(2):75-82.,22 Kurt V, Aras O, Buker N. Comparison of conservative treatment with and without neural mobilization for patients with low back pain: a prospective, randomized clinical trial. J Back Musculoskelet Rehabil. 2020;28. [Epub ahead print].). Notably, approximately 70% of Brazil’s population may have an episode of low back pain during their lifetime(33 Lima ICM, Seguchi HHK, Imamura M, Saito ET, Pinho CP, Imamura ST. Tratamento da lombalgia crônica pela inativação de pontos-gatilho miofasciais - experiência da Divisão de Medicina Física da FMUSP. Acta Fisiátrica. 1999;6(1):10-3.,44 Teixeira MJ, Figueiró JAF, Yeng LT, Pimenta CAM. Tratamento multidisciplinar do doente com dor. Dor um Estudo Multidisciplinar. 1995;62(2):233-40.).
The etiology regarding the development of low back pain is still unclear due to the innumerable factors that may lead to its onset, some of which may be related to repetitive work, pulling and pushing, falls, poor posture, squatting, heavy lifting, muscle imbalance, and compressive syndromes, among others. Chronic pain is among the main causes of absenteeism at work, medical leave, sick leave, workers’ compensation, and low productivity at work(11 Briganó JU, Macedo CSG. Análise da mobilidade lombar e influência da terapia manual e cinesioterapia na lombalgia. Semina: Ciências Biológicas e da Saúde. 2005;26(2):75-82.,55 Loney PL, Stratford PW. The prevalence of low back pain in adults: a methodological review of the literature. Phys Ther. 1999;79(4):384-96.
6 Antonio SF. Abordagem diagnóstica e terapêutica das dores lombares. Rev Bras Med. 2002;59(6):449-61.
7 Teixeira MJ, Teixeira WGJ, Santos FPS, Andrade DCA, Bezerra SL, Figueiró JB, et al. Epidemiologia clínica da dor músculo-esquelética. Rev Med. 2001;80(ed.esp.pt 1):1-21.-88 Neto T, Freitas SR, Marques M, Gomes L, Andrade R, Oliveira R. Effects of lower body quadrant neural mobilization in healthy and low back pain populations: a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;27:14-22.).
It’s important to emphasize that limited mobility of the lumbar spine due to pain can often be associated with this condition(55 Loney PL, Stratford PW. The prevalence of low back pain in adults: a methodological review of the literature. Phys Ther. 1999;79(4):384-96.). Another extremely relevant point regarding spinal nerve injuries, particularly in the lumbar region, is that they are often caused by compressive syndromes such as discal hernias. Such compressions often result in neuropathic pain, which is characterized by spontaneous burning pain, followed by allodynia and hyperalgesia, which can be observed in the nerve pathways of the lower limbs(66 Antonio SF. Abordagem diagnóstica e terapêutica das dores lombares. Rev Bras Med. 2002;59(6):449-61.).
In addition to pharmacological and surgical treatments, there are noninvasive or nonpharmacological treatments, such as physiotherapy. In regard to existing physical therapy treatments, they can lead to the reduction of pain and muscle tension, as well as a possible increase in range of motion. One of the available treatments is neural mobilization (NM), which is characterized by a set of techniques that aim to impose greater tension in the peripheric nervous system through certain postures; slow and rhythmic movements are applied to the peripheral nerves and spinal cord, improving nerve impulse conduction(88 Neto T, Freitas SR, Marques M, Gomes L, Andrade R, Oliveira R. Effects of lower body quadrant neural mobilization in healthy and low back pain populations: a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;27:14-22.
9 Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813(5):878-88.
10 Coppieters MW, Butler DS. In Defense of Neural Mobilization. J Orthop Sports Phys Ther. 2001;31(9):520-1.
11 Cornelson SM, Johnnie ED, Kettner NW. Neural mobilization in a 54-year-old woman with postoperative spinal adhesive arachnoiditis. J Chiropr Med. 2018;17(4):283-8.-1212 Basson A, Olivier B, Ellis R, Coppieters M, Stewart A, Mudzi W. The effectiveness of neural mobilizations in the treatment of musculoskeletal conditions: a systematic review protocol. JBI Database System Rev Implement Rep. 2015;13(1):65-75.).
Studies have demonstrated the beneficial effects of NM, including improved joint pain in patients with rheumatoid arthritis(1313 Lau YN, Ng J, Lee SY, Li LC, Kwan CM, Fan SM, et al. A brief report on the clinical trial on neural mobilization exercise for joint pain in patients with rheumatoid arthritis. Z Rheumatol. 2018;78(5):474-8) and improved cervicobrachial pain(1414 Sanz DR, Solano FU, López DL, Corbalan IS, Morales CR, Lobo CC. Effectiveness of median nerve neural mobilization versus oral ibuprofen treatment in subjects who suffer from cervicobrachial pain: a randomized clinical trial. Arch Med Sci. 2018;14(4):871-9.). NM has demonstrated an excellent prognosis in patients with neuropathic pain, in addition to presenting other advantages such as low operational cost, easy application and no adverse effects.
Results from the previous studies described above show the beneficial effects of NM treatment.
The research questions were:
-
Is NM effective to decrease pain and improve motor behavior on individuals with chronic low back pain?
-
Is NM able to interfere on cytokines modulation?
The objective of this study was to evaluate the effect of NM on individuals with chronic low back pain, as well as analyze possible changes in pain, motor behavior and on cytokine quantification before and after treatment.
METHODS
During the period from July 2016 until September 2017 sixty subjects were screened for eligibility. Sixteen individuals completed the entire study protocol according to the inclusion and exclusion criteria.
Individuals of both sexes who met the following criteria were included in the study: presence of chronic low back pain, radiating or not to one of the lower limbs; age 18 years or older; score ≥ 4 on the visual analog scale (VAS).
Individuals excluded were: suffering from acute low back pain; spondylolisthesis or fibromyalgia; had previous spinal surgery; any sequelae that caused limitations in the range of motion of the lower limb or joint deformity; metal plates, screws, neurological disorders which determine caution in regard to NM; cancer; cognitive disturbances or apparent limitations; any type of pain in other regions that is not characteristic of low back pain; advanced diabetes mellitus; under physiotherapeutic treatment for the same reason; non compensated cardiovascular diseases; significant changes in sensitivity; edema in the lower limbs; and pregnant women.
After eligibility was confirmed, all the procedures to be performed during the study were elucidated, and the subjects signed the Free and Informed Consent Term (FICT), according to Resolution 466/12 of the National Health Council - Brazil, confirming their participation in the research.
After fulfilling the eligibility criteria, a clinical evaluation and assessments of pain intensity, spinal mobility, and hip goniometry were carried out, and a quality of life questionnaire was applied.
Sixteen volunteers participated in this study and were treated with NM technique.
To preserve the accuracy of the intervention effectiveness, participants who missed more than two sessions were excluded from the study. All the subjects were assessed by a blinded evaluator. Both participants and evaluators were encouraged not to discuss the intervention.
Intervention
The NM was performed by the same physiotherapist from the first to the last session on alternate days. Treatment with the technique consists of applying a total of 10 interventions in each patient, with a total duration of 10 minutes, divided into four series of 2 minutes each, with a 30 second interval between each series, according to the protocol proposed in 2012 by the study(1515 Santos FM, Silva JT, Giardini AC, Rocha PA, Achermann AP, Alves AS, et al. Neural mobilization reverses behavioral and cellular changes that characterize neuropathic pain in rats. Mol Pain. 2012;8:57.) and adapted from Butler(1010 Coppieters MW, Butler DS. In Defense of Neural Mobilization. J Orthop Sports Phys Ther. 2001;31(9):520-1.).
The technique was applied with the participant seated in a suitable chair, with a flexed hip (90o) and extended knees. Next, the physiotherapist applied the technique only to the lower limb which presented some impairment due to low back pain, observed in the previous physical examination; in case of absence of pain radiation to any of the limbs, the technique was applied only to the right lower limb, according to the study(1515 Santos FM, Silva JT, Giardini AC, Rocha PA, Achermann AP, Alves AS, et al. Neural mobilization reverses behavioral and cellular changes that characterize neuropathic pain in rats. Mol Pain. 2012;8:57.) (Figure 1).
Representation of the application of neural mobilization
1 – with the patient sitting on a regular chair, the leg to be treated is raised until the lower limb is completely extended; 2 – after adduction followed by internal rotation, extension is continued until the patient experiences some discomfort (not necessarily pain); 3 and 4 – alternation between movements of dorsiflexion and plantar flexion, approximately five times each; 5 and 6 – at the end, the lower limb is elevated and depressed alternately, approximately five times. Steps 3-4 and 5-6 must be alternated until the end of each series of two minutes each.
Sample size
The sample size was calculated based on the VAS for pain, which was considered the primary end point. To this end, the variance reported in the study(1616 Murphy DR, Hurwitz EL, Gregory AA, Clary R. A non-surgical approach to the management of lumbar spinal stenosis: a prospective observational cohort study. BMC Musculoskelet Disord. 2006;7:16.), whose objective was to evaluate NM as a technique for treatment. Considering the mean and standard deviation of the pre-intervention and post-intervention of the present study, with an alpha value (α) of 0.05 and 90%, it was determined that 20 subjects were required for the experimental group.
Outcome measures
First, all personal data from each subject was obtained, including age, occupation and education. After this first step, participants were submitted to two evaluations, one prior to and one at the end of the therapeutic program. Both evaluations assessed quality of life Oswestry Disability Index (ODI), Roland-Morris Disability Questionnaire (RMDQ) and the World Health Organization Quality of Life Questionnaire-bref (WHOQOL-bref), pain intensity, mobility of the lumbar spine and cytokines measures.
Oswestry Disability Index
The ODI Index version 2.0, validated in Portuguese in 2007(1717 Vigatto R, Alexandre NM, Correa Filho HR. Development of a Brazilian Portuguese version of the Oswestry Disability Index: cross-cultural adaptation, reliability, and validity. Spine. 2007;32(4):481-6.), was used. The scale consists of a list of 10 questions with six possible answers. Each answer has a score ranging from zero to 5 in the order in which they are listed, that is, the first value is zero and the last value is 5. The first question assesses pain intensity and the others assess the effect of pain on performance of activities of daily living, such as personal chores, dressing, sleep and so forth(1818 Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25(24):3115-24.).
The total score obtained on this questionnaire was analyzed using a mathematical formula. After adding all the individual’s scores from the questionnaire, the total score as a percentage for each volunteer was calculated. The total score was divided by the number of answered questions multiplied by 5. The result of this division was multiplied by 100, and the final values are given in percentages ([score ÷(number of answered questions × 5)] × 100)(1818 Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25(24):3115-24.).
Roland-Morris Disability Questionnaire
The Portuguese version of the RMDQ was applied to the subjects of the study(1919 Nusbaum L, Natour J, Ferraz MB, Goldenberg J. Translation, adaptation and validation of the Roland-Morris questionnaire - Brazil Roland-Morris. Braz J Med Biol Res. 2001;34(2):203-10.). The questionnaire consists in assessing the severity and level of physical disability induced by low back pain through 24 alternatives with dichotomic answers (yes or no). The questionnaire must be self-filled by the volunteers, demonstrating their success or difficulty in performing their daily life tasks associated with their pain, and the result of the questionnaire is the sum of the positive or marked responses. As some patients had some difficulty reading or understanding the instructions of the questionnaire, the reading was done together with the researchers.
World Health Organization Quality of Life Questionnaire
In order to standardize the evaluation of the patients life quality, the WHOQOL-bref questionnaire was used, which consists of a short and quick application questionnaire developed by the World Health Organization (WHO). The WHOQOL-bref consists of a total of 26 questions, divided into physical, psychological, social relations and environment domains. In order to access the quality of life before and after the proposed treatment, this questionnaire was applied in two periods, the initial measurement (IM), before any treatment, and at final measurement (FM) after the end of 100 sessions of treatment.
This questionnaire was evaluated by the method developed by(2020 Pedroso B, Pilatti LA, Gutierrez GL, Picinin CT. Cálculo dos escores e estatística descritiva do WHOQOL-bref através do Microsoft Excel. RBQV. 2010;2(1):31-6.), a questionnaire analysis that uses Microsoft Excel to identify the means and standard deviations for each individual and unify them in a graph, ranging from zero to 100, and contains all domains analyzed by the questionnaire.
Visual analog scale
The VAS was used for the assessment of pain intensity; it consists of a line ranging from zero to 10, where zero represents the absence of pain and 10 represents the worst pain. After instructions on how to use the scale, volunteers were asked to mark a point on the line that indicated the intensity of pain that they were feeling at the moment of evaluation(2121 Serrano SC. A importância da mensuração da dor na escolha de opióides na dor crônica. âmbito Hosp. 2002;156(1):14-7.).
Mobility of the lumbar spine
Two tests were used to evaluate the mobility of the lumbar spine: the third finger to the ground and goniometry.
The test of the third finger to the ground distance consists of an active test in which the individual is placed in an orthostatic position, with feet separated in line with the hips, keeping the knee extended and heel touching the ground. Then, the participant is asked to perform trunk flexion with the arms extended and to try to bring his hand closer to the ground. Then, using a tape measure, the distance between the tip of the third finger and the ground is measured, and the value in centimeters is considered the mobility of the volunteer’s lumbar spine(11 Briganó JU, Macedo CSG. Análise da mobilidade lombar e influência da terapia manual e cinesioterapia na lombalgia. Semina: Ciências Biológicas e da Saúde. 2005;26(2):75-82.,2222 Puppin MAFL, Marques AP, Silva AG, Futuro Neto HA. Alongamento muscular na dor lombar crônica inespecífica: uma estratégia do método GDS. Fisioter Pesqui. 2011;18(2):116-21.).
Goniometry refers to the measurement of individuals’ joint angles; it was applied before the first session and after the last session of NM. To minimize measurement error, the physiotherapist in charge underwent training. Goniometric measurements of the hip joint of the participants in this study were used for both thigh flexion; the amplitude varies between zero - 131º±6.4º, and the articular range varies from zero to 13º±5.4º; measurements may vary from individual to individual more or less within these established values(2323 Zhang JM, An J. Cytokines, inflammation and pain. Int Anesthesiol Clin. 2007;45(2):27-37.).
Cytokines measurements
Blood was collected from each group to evaluate the possible impact of the technique on pro- and anti-inflammatory cytokines. Two collections were performed: the initial measurement (I) and the final measurement after the last session (F) of treatment. To evaluate cytokine concentration, the blood serum of the individuals was used for these analyses.
For specific IL-1β, IL-4, IL-6, and TNF-α cytokines, specific reagents contained in the Milliplex®TM Map kit (Millipore Corporation, Darmstadt-Germany) were assessed by Multiplex (Enzyme-Linked Immunosorbent Assay) according to the protocol specified by the manufacturer.
All the study procedures were conducted in accordance with the Ethics Committee involving humans of the Universidade de São Paulo Instituto de Ciências Biomédicas - São Paulo, Brazil (CAAE: 56978016.1.0000.5467). The trial was also registered in Clinical Trials (clinicaltrials.gov - NCT02671409).
Statistical analysis
Results are presented as the mean±SEM. Statistical analyses of data were generated using GraphPad Prism, version 5 (Graph-Pad Software Inc., San Diego, CA). Statistical comparison was performed using a paired t-test. In all cases, p<0.05 was considered statistically significant.
RESULTS
In figure 2 shows the characterization the study’s subjects. Sixty subjects were screened for eligibility and only 16 individuals completed the entire study protocol according to the inclusion and exclusion criteria. From those 16 individuals, 8 were Men and 8 Women, with age between 25 to 45 years old.
Oswestry Disability Index
After the initial measurement of ODI, the mathematical formula was applied to evaluate the degree of incapacity of the individuals. In the initial measure (I), the ODI can be classified into five levels or stages of disability. The first level, between zero and 20%, characterizes a minimal disability associated with the activities. The second stage, between 21 and 40%, characterizes a moderate disability. The interval between 41 and 60% characterizes a severe disability, and the interval between 61 and 80% characterizes crippling back pain. Finally, the interval between 81 and 100% characterizes bed bound immobility.
Regarding the patients that participated in the present study, one was in level 4 and one in level 3, with a high level of disability, and the other patients had an average score between stages 2 and 1, with moderate disability. In the final measure (F) of the ODI questionnaire, the effect of treatment on changes in clinical condition after application of the mathematical formula was evaluated. Comparing the initial (I) and final (F) measurements of ODI, an improvement on the clinical condition in all subjects was observed; many of the individuals analyzed after the treatment obtained an excellent response with the proposed protocol. All patients decreased in disability by one stage, and by the end of the program almost all subjects reached the first stage, in the range of 0 to 20%, which classifies the change as excellent (Table 1).
Analysis of the results obtained in the initial (I) and final (F) measurements on the Oswestry Disability Index, before and after the proposed treatment
Roland-Morris Disability Questionnaire
In this questionnaire, positive answers and a value equal to or lower than 10 points indicates that the person with low back pain presents a small level of disability, that is, despite the pain, there is no impediment of daily life tasks. When the total varies between 11 and 14 alternatives indicated as positive, mild or moderate inability to perform daily activities is present. When the positive responses are equal to or greater than 15, the individual has severe disability.
In the initial measurement, 14 individuals presented the normal parameter, not showing any kind of incapacity in performing daily life activities. In the initial measurement, two individuals from the same group presented severe incapacity to perform daily activities. At the end of treatment, this questionnaire was reapplied, and 15 of the subjects presented normal parameters, while one of the individuals with severe disability returned to normal levels; the other individual who also presented severe level of disability partially reversed their condition, reaching mild/moderate disability when performing daily activities(Table 2).
Analysis of the results obtained in the initial (I) and final (F) measurements on Roland-Morris Disability Questionnaire (RMDQ), before and after the proposed treatment
World Health Organization Quality of Life
In the WHOQOL-bref questionnaire an important reduction, mainly in the physical and environment domain, when comparing before and after treatment, was observed. In the psychological and social relations domains, no changes during the analyzed period were observed (Figure 3).
Analysis of the results obtained in the initial and final measurements on the WHOQOL-bref questionnaire.
The symbols represent the statistically significant difference between values prior and after treatment for each domain * p<0.05.
Pain intensity
As shown in figure 4, when the means obtained for each period were analyzed, the initial score (I) was 7.16 for the VAS, indicating moderate intensity pain. Beginning with the second intervention session with the NM, a statistically significant difference was already observed in relation to the initial measurement (I) until the final treatment (F) (*p<0.001). On the final measure, that is, after 10 sessions of NM, the individuals presented a score equal to 1.61 for the VAS, nearly the lowest score possible on the scale. Therefore, it is suggested that the NM was able to reduce the pain intensity of individuals with chronic low back pain by approximately 70% compared to initial pain intensity.
Pain intensity measured by visual analog scale
(I=initial measure), during (s = sessions) and after (F=final measure) treatment with NM (n=18). The symbols represent the statistically significant difference between times analyzed and initial measure * p<0.0001. Data is presented as the mean±SEM.
Mobility of lumbar spine:
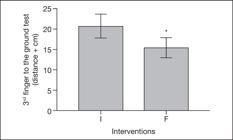
Third finger to the ground test:
Before treatment, in the initial measurement (I), individuals’ average pretreatment distance to the ground was 20.67cm. Subsequently, these same individuals started treatment with the NM. At the end of the 10 interventions of NM treatment (final measurement F), the mobility of the lumbar spine test was performed again to ascertain the effectiveness of the treatment, and a mean of 15.4 cm distance to the ground was obtained. This improvement was statistically significant for lumbar spine mobility after treatment according to the protocol (*p<0.04). This result leads us to suggest that the NM could improve the lumbar mobility of individuals with chronic low back pain by approximately 25.5% (Figure 5).
Mobility of the lumbar spine by the third finger to the ground test
I - measurement initial; F = measurement final.
Lumbar spine mobility before (I=initial measure) and after (F=final measure) treatment. The symbols represent the statistically significant difference between groups * p<0.04. Data is presented as the mean±SEM.
Hip goniometry
Before treatment, a mean hip flexion of 87.92º, measured by hip flexion in dorsal decubitus, as shown in figure 6A, was observed. Subsequently, the subjects started treatment with the NM. At the end of treatment, a final measurement (F) was performed to ascertain the effectiveness of the treatment. At the end of the 10 interventions with the NM technique, an average of 98.57º of hip flexion was observed. This improvement was statistically significant for goniometry after treatment with the proposed protocol (*p<0.04).
Goniometry of hip flexion (A) and hip extension (B)
Before (I=initial measure) and after (F=final measure) treatment. The symbols represent the statistically significant difference between groups * p<0.04. Data is presented as the mean±SEM.
Additionally, regarding measurement of hip extension in the ventral decubitus, as shown in figure 6B, on initial measurement (I), observed an average of 13.8º of hip extension was observed. At the end of treatment, a mean hip extension of 18.2º was obtained. This improvement was statistically significant for goniometry after treatment with the proposed protocol (*p<0.04).
Cytokines
Regarding the cytokine assay, the involvement of pro- and anti-inflammatory cytokines (Figure 7) was evaluated. In relation to pro-inflammatory cytokines, IL-1β, IL-6, and TNF-α before and after the last session of NM treatment were analyzed. The results show that there was a statistically significant decrease in IL-1β and TNF-α concentrations (Figures 7A and B, respectively) between the initial (I) and final (F) means, that is, before and after the application of the treatment protocol.
Concentration of cytokines IL-1β (A), FTN-α (B), IL-6 (C) and IL-4 (D).
Measurement before- initial (I) and after-final (F) NM treatment. The symbols represent the statistically significant difference between groups; * p<0.04. Data is presented as the mean ± SEM.
Furthermore, analysis of the cytokine IL-6, which is considered a pro-inflammatory and modulatory cytokine, showed a statistically significant increase at the final measurement (F) compared to the initial measurement (before NM treatment) (*p<0.009) (Figure 7C). Analysis of the anti-inflammatory cytokine IL-4 (Figure 7D) revealed a significant difference before (I) and after (F) the application of treatment, that is, an increase in this cytokine after treatment (* p<0.03).
DISCUSSION
Low back pain can lead to disability over time and represents an important economic impact(2424 Nee RJ, Butler D. Management of peripheral neuropathic pain: Integrating neurobiology, neurodynamics, and clinical evidence. Phys Ther Sport. 2006;7(1):36-49.,2525 Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386(9995):743-800.).
Based on the present study results, it’s suggest that the NM technique, when applied in individuals with chronic low back pain, either alone or combined with pharmacological therapy, is able to improve quality of life, reduce pain intensity, increase functional mobility, as well as provide a huge decrease in pro-inflammatory cytokines.
The ODI questionnaire was used to measure the disability level for all subjects. Although patients were mostly classified at the stage two level of disability before applying the technique, a reduction in the level of disability of all subjects was observed after application of the protocol. Furthermore, success in improving the quality of life of all study patients was achieved.
The RMDQ is used to analyze the level of physical disability induced by low back pain. In the present work, it’s suggested that the proposed protocol was able to improve disability of almost all treated individuals from mild to normal.
Important improvement in quality of life according to the WHOQOL-bref questionnaire was also observed. The treatment was able to improve the physical domain after the last session of NM treatment. This domain includes the perception of pain and discomfort in the patients’ lives, and is associated with other factors such as fatigue, mobility and sleep. Regarding environment domain, there was a reduction in the final measure compared to initial measure, but this difference is attributed to the interpretation of individuals before the analyzed questions. No difference was observed in the psychological and social relations domain between the two periods where the questionnaire was applied. These data corroborate the data found by the study(2626 Stefane T, Santos AM, Marinovic A, Hortense P. Dor lombar crônica: Intensidade de dor, incapacidade e qualidade de vida. Acta Paul Enferm. 2013;26(1):14-20.), whose authors observed, using the WHOQOL-bref questionnaire, that the physical domain was the most intensely altered, and suggested that this change was strongly associated with the individuals’ level of disability.
Regarding the pain scale, significant improvement in the pain of patients treated with the NM technique was observed. All individuals had significant improvement, an average of 70% reduction in pain after the treatment, evaluated by the VAS. The present study results corroborate authors who observed improvement in pain in all individuals with sciatic nerve injury(2727 Rittner HL, Brack A, Stein C. The other side of the medal: how chemokines promote analgesia. Neurosci Lett. 2008;437(3):203-8.) and low back pain(22 Kurt V, Aras O, Buker N. Comparison of conservative treatment with and without neural mobilization for patients with low back pain: a prospective, randomized clinical trial. J Back Musculoskelet Rehabil. 2020;28. [Epub ahead print].,88 Neto T, Freitas SR, Marques M, Gomes L, Andrade R, Oliveira R. Effects of lower body quadrant neural mobilization in healthy and low back pain populations: a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;27:14-22.).
The present work also corroborates findings obtained by by the sudies(2424 Nee RJ, Butler D. Management of peripheral neuropathic pain: Integrating neurobiology, neurodynamics, and clinical evidence. Phys Ther Sport. 2006;7(1):36-49.,2828 Sweeney J, Harms A. Persistent mechanical allodynia following injury of the hand. Treatment through mobilization of the nervous system. J Hand Ther. 1996;9(4):328-38.), who observed a reversal of allodynia and hyperalgesia and an improvement in the range of motion of the affected limb after the NM technique.
When the functional capacity of all patients was analyzed, an improvement in their mobility was observed. A statistically significant improvement in the mobility of the lumbar spine, evaluated through the third finger distance and the hip goniometry evaluation tests, was observed. Results showed an average of 25% increase in lumbar spine mobility, a large and statistically significant improvement after treatment. An improvement in the joint angles of the individuals treated with NM for both flexion and extension was also observed. This improvement was approximately 24.17% for extension and 10.8% for flexion.
It should be mentioned that the authors also observed improvement in patients’ mobility using the Shöber’s test, another similar clinical test to assess lumbar mobility. Recent studies also observed statistically significant improvement in lumbar mobility in individuals treated with NM after sciatic nerve injury(2929 Barbosa APB, Leal SS. Analysis of the efficacy of neural mobilization of the sciatic nerve in improving ROM. ConScientiae Saúde. 2015;14(3):463-9.) or after low back pain(88 Neto T, Freitas SR, Marques M, Gomes L, Andrade R, Oliveira R. Effects of lower body quadrant neural mobilization in healthy and low back pain populations: a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;27:14-22.).
Since improvement in patients’ pain severity and motor status associated with the NM technique was observed, serum concentration of cytokines was then evaluated. It is already known that pro-inflammatory cytokines are involved in hyperalgesia and allodynia generation due to compressive syndromes. Studies have already demonstrated an increase in pro-inflammatory cytokines in the blood and tissues of individuals and animals with neuropathic and chronic pain(3030 Cui JG, Holmin S, Mathiesen T, Meyerson BA, Linderoth B. Possible role of inflammatory mediators in tactile hypersensitivity in rat models of mononeuropathy. Pain . 2000;88(3):239-48.).
The present study results demonstrated a decrease in pro-inflammatory cytokines and an increase in anti-inflammatory cytokines after NM treatment. A decrease in IL-1β and TNF-α and an increase in IL-4 pro- and anti-inflammatory cytokines was observed. Results corroborate previous studies showing an increase in plasma pro-inflammatory cytokines in patients with neuropathic pain(3232 Kraychete DC, Sakata RK, Issy AM, Bacellar O, Jesus RS, Carvalho EM. Proinflammatory cytokines in patients with neuropathic pain treated with tramadol. Braz J Anesthesiol. 2009;59(3):297-303.) and a reduction in the concentration of pro-inflammatory cytokines (IL-1β and TNF-α) after treatment of animals with the NM(3333 Zhu GC, Tsai KL, Chen YW, Hung CH. Neural mobilization attenuates mechanical allodynia and decreases proinflammatory cytokine concentrations in rats with painful diabetic neuropathy. Phys Ther. 2018;98(4):214-22.).
Regarding IL-6, an increase in this cytokine after treatment was observed. This cytokine is also characterized as a pro-inflammatory and modulator cytokine. Some studies show that IL-6, along with IL-1β and TNF-α, may stimulate the synthesis of pro-inflammatory cytokine receptors and opioids in the posterior root ganglion, leading to a dual effect,(99 Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813(5):878-88.,2323 Zhang JM, An J. Cytokines, inflammation and pain. Int Anesthesiol Clin. 2007;45(2):27-37.,2727 Rittner HL, Brack A, Stein C. The other side of the medal: how chemokines promote analgesia. Neurosci Lett. 2008;437(3):203-8.,3131 Puehler W, Zöllner C, Brack A, Shaqura MA, Krause H, Schäfer M, et al. Rapid upregulation of µ opioid receptor mRNA in dorsal root ganglia in response to peripheral inflammation depends on neuronal conduction. Neuroscience. 2004;129(2):473-9.).
It is well known that, in clinical practice, difficulty to treat neuropathic pain has been highly evidenced, due to the inadequate understanding of the cellular and molecular mechanisms involved in the development and/or maintenance of this kind of pain. Based on the present study findings, the model may be of great value, as this technique is non-invasive, since it was able to reduce pro-inflammatory cytokines and increase anti-inflammatory cytokine.
Based on the present study results and the results in the literature, it’s possible to say that NM technique can decrease pain intensity and improve functional capacity, demonstrating its importance for clinical practice. NM can also be suggested as a possible treatment for individuals with low back pain, since no side effects were observed during the month-long treatment. Using this model together with physicians to treat patients with this type of pain is recommended, improving patients’ quality of life and, consequently, reducing the use of drugs.
Limitations of this study
Limitations regarding regarding the recruitment and maintenance of patients to adhere the treatment were encountered, since most showed a rapid improvement in their initial condition, abandoning treatment before its end. Another limitation is the treatment schedule of three times a week, which can coincide with the patients obligations and work hours. Another limitation foreseen by the study is that the individuals to be recruited for treatment must have a level of education which allows them to read, interpret and answer the quality of life questionnaires. All the limitations listed above do not prevent the work from being carried out, however, they have limited the number of individuals who are able to be recruited for treatment.
CONCLUSION
The treatment with NM implemented in the present study reduced the pain intensity and increased the lumbar mobility of individuals with chronic low back pain, which in general accelerated the process of improvement/recovery of the functional capacity of these individuals and accelerated their return to activities of normal daily life.
Furthermore, the protocol used in the study significantly improved the patients’ quality of life and indicated a change in concentration of pro and anti-inflammatory cytokines at the end of treatment with NM in individuals with chronic low back pain.
It’s worth noting that the NM can also be combined with other noninvasive conventional treatments, such as pharmacological treatment, which also makes it a coadjutant tool in the treatment of chronic low back pain.
-
Sponsoring sources: FAPESP 2017/05218-5
ACKNOWLEDGMENTS
We would like to thank Kelle Vanessa de Oliveira Carvalho and Mirian Cristina Rocha for their help in anamnesis of patients.
REFERENCES
-
1Briganó JU, Macedo CSG. Análise da mobilidade lombar e influência da terapia manual e cinesioterapia na lombalgia. Semina: Ciências Biológicas e da Saúde. 2005;26(2):75-82.
-
2Kurt V, Aras O, Buker N. Comparison of conservative treatment with and without neural mobilization for patients with low back pain: a prospective, randomized clinical trial. J Back Musculoskelet Rehabil. 2020;28. [Epub ahead print].
-
3Lima ICM, Seguchi HHK, Imamura M, Saito ET, Pinho CP, Imamura ST. Tratamento da lombalgia crônica pela inativação de pontos-gatilho miofasciais - experiência da Divisão de Medicina Física da FMUSP. Acta Fisiátrica. 1999;6(1):10-3.
-
4Teixeira MJ, Figueiró JAF, Yeng LT, Pimenta CAM. Tratamento multidisciplinar do doente com dor. Dor um Estudo Multidisciplinar. 1995;62(2):233-40.
-
5Loney PL, Stratford PW. The prevalence of low back pain in adults: a methodological review of the literature. Phys Ther. 1999;79(4):384-96.
-
6Antonio SF. Abordagem diagnóstica e terapêutica das dores lombares. Rev Bras Med. 2002;59(6):449-61.
-
7Teixeira MJ, Teixeira WGJ, Santos FPS, Andrade DCA, Bezerra SL, Figueiró JB, et al. Epidemiologia clínica da dor músculo-esquelética. Rev Med. 2001;80(ed.esp.pt 1):1-21.
-
8Neto T, Freitas SR, Marques M, Gomes L, Andrade R, Oliveira R. Effects of lower body quadrant neural mobilization in healthy and low back pain populations: a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;27:14-22.
-
9Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813(5):878-88.
-
10Coppieters MW, Butler DS. In Defense of Neural Mobilization. J Orthop Sports Phys Ther. 2001;31(9):520-1.
-
11Cornelson SM, Johnnie ED, Kettner NW. Neural mobilization in a 54-year-old woman with postoperative spinal adhesive arachnoiditis. J Chiropr Med. 2018;17(4):283-8.
-
12Basson A, Olivier B, Ellis R, Coppieters M, Stewart A, Mudzi W. The effectiveness of neural mobilizations in the treatment of musculoskeletal conditions: a systematic review protocol. JBI Database System Rev Implement Rep. 2015;13(1):65-75.
-
13Lau YN, Ng J, Lee SY, Li LC, Kwan CM, Fan SM, et al. A brief report on the clinical trial on neural mobilization exercise for joint pain in patients with rheumatoid arthritis. Z Rheumatol. 2018;78(5):474-8
-
14Sanz DR, Solano FU, López DL, Corbalan IS, Morales CR, Lobo CC. Effectiveness of median nerve neural mobilization versus oral ibuprofen treatment in subjects who suffer from cervicobrachial pain: a randomized clinical trial. Arch Med Sci. 2018;14(4):871-9.
-
15Santos FM, Silva JT, Giardini AC, Rocha PA, Achermann AP, Alves AS, et al. Neural mobilization reverses behavioral and cellular changes that characterize neuropathic pain in rats. Mol Pain. 2012;8:57.
-
16Murphy DR, Hurwitz EL, Gregory AA, Clary R. A non-surgical approach to the management of lumbar spinal stenosis: a prospective observational cohort study. BMC Musculoskelet Disord. 2006;7:16.
-
17Vigatto R, Alexandre NM, Correa Filho HR. Development of a Brazilian Portuguese version of the Oswestry Disability Index: cross-cultural adaptation, reliability, and validity. Spine. 2007;32(4):481-6.
-
18Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25(24):3115-24.
-
19Nusbaum L, Natour J, Ferraz MB, Goldenberg J. Translation, adaptation and validation of the Roland-Morris questionnaire - Brazil Roland-Morris. Braz J Med Biol Res. 2001;34(2):203-10.
-
20Pedroso B, Pilatti LA, Gutierrez GL, Picinin CT. Cálculo dos escores e estatística descritiva do WHOQOL-bref através do Microsoft Excel. RBQV. 2010;2(1):31-6.
-
21Serrano SC. A importância da mensuração da dor na escolha de opióides na dor crônica. âmbito Hosp. 2002;156(1):14-7.
-
22Puppin MAFL, Marques AP, Silva AG, Futuro Neto HA. Alongamento muscular na dor lombar crônica inespecífica: uma estratégia do método GDS. Fisioter Pesqui. 2011;18(2):116-21.
-
23Zhang JM, An J. Cytokines, inflammation and pain. Int Anesthesiol Clin. 2007;45(2):27-37.
-
24Nee RJ, Butler D. Management of peripheral neuropathic pain: Integrating neurobiology, neurodynamics, and clinical evidence. Phys Ther Sport. 2006;7(1):36-49.
-
25Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386(9995):743-800.
-
26Stefane T, Santos AM, Marinovic A, Hortense P. Dor lombar crônica: Intensidade de dor, incapacidade e qualidade de vida. Acta Paul Enferm. 2013;26(1):14-20.
-
27Rittner HL, Brack A, Stein C. The other side of the medal: how chemokines promote analgesia. Neurosci Lett. 2008;437(3):203-8.
-
28Sweeney J, Harms A. Persistent mechanical allodynia following injury of the hand. Treatment through mobilization of the nervous system. J Hand Ther. 1996;9(4):328-38.
-
29Barbosa APB, Leal SS. Analysis of the efficacy of neural mobilization of the sciatic nerve in improving ROM. ConScientiae Saúde. 2015;14(3):463-9.
-
30Cui JG, Holmin S, Mathiesen T, Meyerson BA, Linderoth B. Possible role of inflammatory mediators in tactile hypersensitivity in rat models of mononeuropathy. Pain . 2000;88(3):239-48.
-
31Puehler W, Zöllner C, Brack A, Shaqura MA, Krause H, Schäfer M, et al. Rapid upregulation of µ opioid receptor mRNA in dorsal root ganglia in response to peripheral inflammation depends on neuronal conduction. Neuroscience. 2004;129(2):473-9.
-
32Kraychete DC, Sakata RK, Issy AM, Bacellar O, Jesus RS, Carvalho EM. Proinflammatory cytokines in patients with neuropathic pain treated with tramadol. Braz J Anesthesiol. 2009;59(3):297-303.
-
33Zhu GC, Tsai KL, Chen YW, Hung CH. Neural mobilization attenuates mechanical allodynia and decreases proinflammatory cytokine concentrations in rats with painful diabetic neuropathy. Phys Ther. 2018;98(4):214-22.
Publication Dates
-
Publication in this collection
19 June 2020 -
Date of issue
Jul-Sep 2020
History
-
Received
18 Feb 2020 -
Accepted
25 May 2020