ABSTRACT
Acute suppurative thyroiditis is a very rare and life-threatening endocrine emergency. Thyrotoxicosis is a rare condition accompanying acute suppurative thyroiditis. While the majority of the cases in the literature are caused by different reasons, spontaneous development is very rare. We present a patient with acute suppurative thyroiditis who presented to our clinic with thyrotoxic findings, and we compared the case to the literature. A 31-year-old male patient was admitted to our clinic with a complaint of progressive neck pain, swelling and redness on midline neck, fever, and palpitations. On physical examination, swelling, redness and tenderness were detected on the neck region that was consistent with the thyroid location. He presented with tremor on the hands, tachycardia and agitation. Thyroid function tests were compatible with thyrotoxicosis, but there were findings supporting the presence of infection in biochemistry tests. On his radiological evaluations, a heterogeneous lesion divided with small septs was observed, with consolidation areas in the left thyroid lobe. In fine needle aspiration biopsy, 2mL of purulent fluid could be aspirated due to the presence of small, separated consolidation areas. He initiated on antibiotic therapy, propranolol, steroid and symptomatic treatment. Eikenella corrodens was detected on the culture antibiogram. Antibiotic therapy was continued for 14 days due to less symptoms and better biochemical values. After treatment, the patient had normal thyroid function, had relief of fever and redness of the neck, and was followed-up. It should be kept in mind that acute suppurative thyroiditis may develop spontaneously with the findings of thyrotoxicosis, with no risk factors.
Thyroiditis; Thyrotoxicosis; Eikenella corrodens; Neck
RESUMO
A tireoidite supurativa aguda é uma emergência endócrina muito rara e com risco de vida. A tireotoxicose é uma doença rara, que acompanha a tireoidite supurativa aguda. A maioria dos casos descritos na literatura tem diferentes causas, mas o desenvolvimento espontâneo é muito raro. Relatamos o caso de um paciente com tireoidite supurativa aguda, que veio a nossa clínica apresentando achados tireotóxicos, e o comparamos com a literatura. Trata-se de paciente do sexo masculino, 31 anos, que foi internado em nossa clínica com queixa de dor progressiva, edema e vermelhidão na linha média do pescoço, febre e palpitações. Ao exame físico, foram observados edema, vermelhidão e sensibilidade à dor na região do pescoço, consistente com a localização da tireoide. Apresentava tremor de mãos, taquicardia e agitação. Embora os exames de função tireoidiana fossem compatíveis com tireotoxicose, houve achados que sustentavam a presença de infecção nos exames bioquímicos. Nas avaliações radiológicas, observou-se lesão heterogênea dividida por pequenos septos, com áreas de consolidação no lobo tireoidiano esquerdo. Na biópsia por aspiração por agulha fina, foi possível aspirar apenas 2mL de líquido purulento, devido à presença de pequenas áreas de consolidação separadas umas das outras. Iniciaram-se antibioticoterapia, administração de propranolol e esteroides, além de tratamento sintomático. Eikenella corrodens cresceu na cultura do antibiograma. A antibioticoterapia foi estendida por 14 dias devido à melhora nos sintomas e dos valores bioquímicos. Após o tratamento, o paciente se apresentava eutireoideo, com melhora na febre e na vermelhidão no pescoço, sendo então acompanhado. Deve-se ter em mente que a tireoidite supurativa aguda pode se desenvolver espontaneamente com achados de tireotoxicose, sem nenhum fator de risco.
Tireoidite; Tireotoxicose; Eikenella corrodens; Pescoço
INTRODUCTION
Acute suppurative thyroiditis (AST) is an extremely rare and life-threatening endocrine emergency, with an incidence of 0.1% to 0.7% in all thyroid diseases.(11. Al-Dajani N, Wootton SH. Cervical lymphadenitis, suppurative parotitis, thyroiditis, and infected cysts. Infect Dis Clin North Am. 2007;21(2):523-41, viii. Review.) Thyroid hormone levels are generally normal in AST, but thyrotoxicosis is a rare condition.(22. Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003; 348(26):2646-55. Review. Erratum in: N Engl J Med. 2003;349(6):620.)Generally, AST develops secondary to systemic diseases, immunodeficiency conditions or traumatic events, such as fine needle aspiration (FNAB), whereas spontaneous AST is quite rare.(22. Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003; 348(26):2646-55. Review. Erratum in: N Engl J Med. 2003;349(6):620.) In this case report, we aimed to discuss a patient who presented with thyrotoxic symptoms to our clinic, and was diagnosed with spontaneous AST.
CASE REPORT
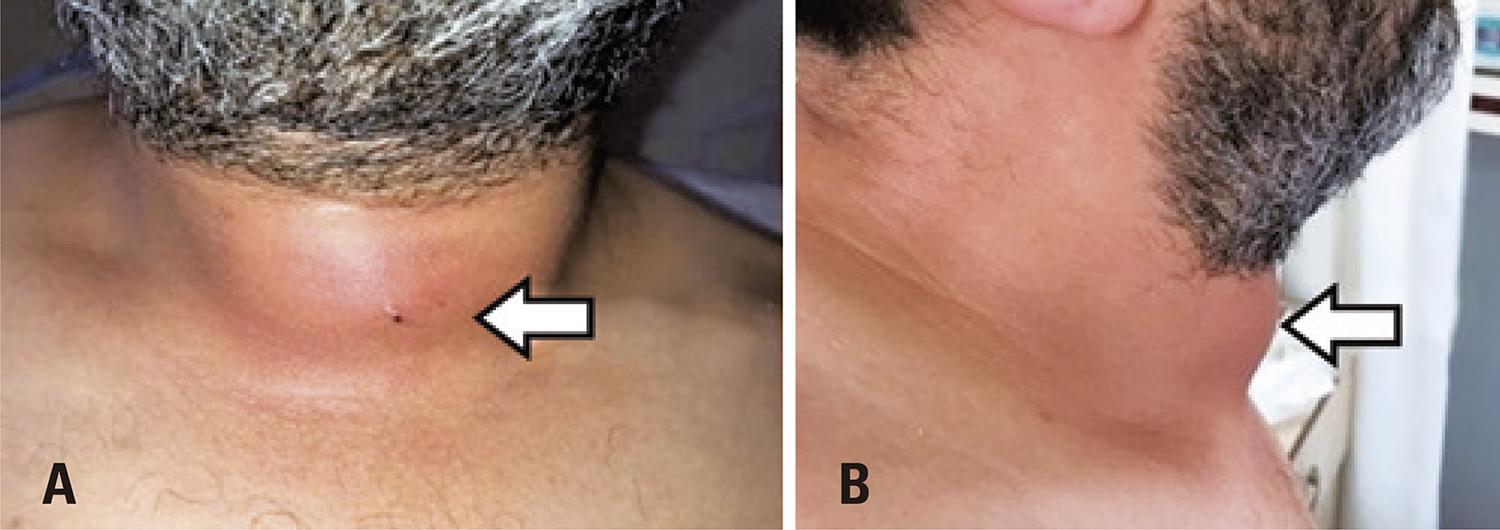
A 31-year-old male patient without any history of chronic diseases, thyroid pathologies or previous neck surgery, was admitted to the ear-nose-throat outpatient clinic with the complaints of neck pain, dysphagia, swelling and redness on midline neck region, fever, and palpitations that started 10 days ago. He had tremor on hands and was generally agitated. The patient had no history of neck trauma and his medical history and family history were uneventful. Blood pressure was 120×70mmHg, axillary temperature 38.5°C, pulse rate 120/minute, respiratory rate 16/minute, and oxygen saturation was 99%. Otolaryngology examination revealed swelling, redness, and tenderness of approximately 7cm, especially in the area corresponding to the thyroid region (Figure 1). In his systemic examination, breath sounds were normal, tachycardia was present, but no pathological sounds or murmurs were detected. In the endoscopic examination, the patient’s nasopharynx, oropharynx, and larynx examinations were normal and there was no fistula in the pyriform sinuses. The other otolaryngology examinations were normal. The patient presented with tremor on the hands and was agitated. Sinus tachycardia was present in the electrocardiogram. In laboratory examinations white blood cell count was 13,200 (75% neutrophil); hemoglobin 15.2g/dL; erythrocyte sedimentation rate (ESR) 54mm/hour; C-reactive protein (CRP) 152mg/L; and liver function tests were minimally elevated. With the suspicion of thyroid diseases, thyroid function tests were analyzed and thyroid-stimulating hormone (TSH) was 0.01µIU/mL (0.38µIU/mL to 5.33µIU/mL), free T4 was 4.9ng/dL (0.58ng/dL to 1.6ng/dL), free T3 was 13.27pg/mL (2.66pg/mL to 4.37pg/mL). These tests showed the patient had thyrotoxicosis.
Appearance of the patient’s neck upon admission. (A) Anterior view of the patient’s neck; and (B) Lateral view of the patient’s neck. White arrow: redness, painful swelling of the thyroid
Anti-thyroglobuline and anti-thyroperoxidase antibodies were negative. Immunoglobulin values were normal. Neck and thyroid ultrasound showed a heterogeneous lesion of 33×34×66mm in left thyroid lobe, formed by septated cystic components, and no robust thyroid parenchyma was seen in the left lobe. In the left anterior neck region, there were compartments with cystic echogenicity on the skin, subcutaneous tissue and thyroid region, while the right thyroid gland parenchyma was normal (Figure 2). The patient was hospitalized.
Neck ultrasound of the patient. (A) Axial ultrasound image of thyroid right lobe and isthmus of the patient. The right lobe appears to be normal (B) Axial ultrasound image of the left lobe of the patient. A heterogeneous lesion composed of septated cystic component, intact thyroid parenchyma is not present in the left lobe. Compartments in cystic echogenicity are observed in the left anterior region of the neck, on skin, subcutaneous tissue, and thyroid lobes
RL: right lobe; is: isthmus; T: trachea; LB: left lobe.
Neck computed tomography with no contrast enhancement revealed a heterogeneous, hypodense lesion, containing some areas of necrotic-liquid density, 65×60×65mm in size, located on the left lobe, along the isthmus level and extending from the midline to the right lobe (Figure 3). Due to the presence of multiple small areas with several septations, only 2mL of purulent fluid could be aspirated in FNAB, and the material was sent for culture antibiogram.
Axial (A), sagittal (B) and coronal (C) non-contrast computed tomography images of the patient. There is a heterogeneous, hypodense lesion located on the left lobe through the isthmus level, and the necrotic-fluid density areas extending from the midline to the right lobe (white arrow)
An: anterior; R: right side.
Empirically, treatment was initiated with ampicillin/sulbactam (1,500mg, four times a day, intravenous; Sulcid, İbrahim Etem-Menarini, Istanbul, Turkey) and ornidazole (500mg, twice a day, intravenous; Orniject, Tüm Ekip İlaç, Istanbul, Turkey) for infection. Propranolol hydrochloride (20mg, twice a day, PO; Dideral, Sanofi, Istanbul, Turkey) was started for patient’s agitation, tremor and palpitations. Methylprednisolone (40mg a day, intravenous; Prednol-L, Mustafa Nevzat Pharmaceuticals, Istanbul, Turkey) was started for inflammation of thyroid gland and dexketoprofen trometamol (100mg a day, intravenous; Arveles, İbrahim Etem – Menarini Group, Istanbul, Turkey) for pain and inflammation. Methimazole (5mg, three times a day, PO; Thyromazol, Abdi İbrahim İlaç, Istanbul, Turkey) was prescribed for thyrotoxicosis, as an antithyroid drug.
In culture antibiogram showed Eikenella corrodens, susceptible to ampicillin. Ornidazole was discontinued and the treatment was continued with ampicillin/sulbactam. On the 5th day of the treatment, TSH was 0.003µIU/mL, freeT4 3.61ng/dL, freeT3 4.32pg/mL, ESR 35mm/hour, and CRP was 8mg/L. Ampicillin-sulbactam treatment was continued for 14 days, then TSH was 0.01µIU/mL, freeT4 1.14ng/dL, freeT3 2.90pg/mL, ESR 8mm/hour, and CRP was 6mg/L. These findings showed that the patient’s infection was regressing and thyrotoxicosis was getting better.
The patient was discharged 17 days after hospitalization, since he had a complete regression of agitation, tremor, palpitations and painful redness on the neck. Thyroid function tests, ESR and CRP levels were normal at the first month after treatment. The patient was followed as euthyroid in the first year after treatment.
DISCUSSION
Because of the high vascularization and lymphatic drainage, high iodine concentration and encapsulation, the thyroid gland is resistant to infections and acute thyroid gland infections are extremely rare.(22. Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003; 348(26):2646-55. Review. Erratum in: N Engl J Med. 2003;349(6):620.)Acute suppurative thyroiditis may develop due to direct extension of adjacent regions, retropharyngeal abscess, penetrating traumas, thyroid FNAB, intravenous drug usage, rupture or perforation of esophagus, or secondary infections due to immunosuppressive diseases.(11. Al-Dajani N, Wootton SH. Cervical lymphadenitis, suppurative parotitis, thyroiditis, and infected cysts. Infect Dis Clin North Am. 2007;21(2):523-41, viii. Review.,22. Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003; 348(26):2646-55. Review. Erratum in: N Engl J Med. 2003;349(6):620.)Pyriform sinus fistula is a rare condition which is resulting from failure of intrauterine obliteration of third and fourth branchial arch embriologically. The tract of this sinus courses from the pyriform sinus to the thyroid gland, into the perithyroid tissue. The opening of the pyriform sinus fistula can cause AST, especially in the left thyroid lobe.(33. Pereira KD, Losh GG, Oliver D, Poole MD. Management of anomalies of the third and fourth branchial pouches. Int J Pediatr Otorhinolaryngol. 2004; 68(1):43-50.
4. Paes JE, Burman KD, Cohen J, Franklyn J, McHenry CR, Shoham S, et al. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid. 2010;20(3):247-55. Review.-55. Kondo T. Acute suppurative thyroiditis secondary to pyriform sinus fistula. Lancet Infect Dis. 2019;19(4):447.) The spontaneous development of AST is very rare. In our case, pyriform sinus examination was normal, no brachial cyst was observed. Additionally, the patient had no risk factors for developing AST.
Generally, patients who had AST present with neck swelling, redness of the neck, pain, dysphagia and fever.(22. Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003; 348(26):2646-55. Review. Erratum in: N Engl J Med. 2003;349(6):620.) Differential diagnosis should be made in these patients, especially with subacute thyroiditis and thyroid malignancies, as well as thyroid cyst rupture, sternocleidomastoid abscess and deep vein thrombosis. During the examination, the patient should be monitored quickly and the vital signs should be closely monitored.(11. Al-Dajani N, Wootton SH. Cervical lymphadenitis, suppurative parotitis, thyroiditis, and infected cysts. Infect Dis Clin North Am. 2007;21(2):523-41, viii. Review.,22. Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003; 348(26):2646-55. Review. Erratum in: N Engl J Med. 2003;349(6):620.)Our patient had no previous history of thyroid malignancy, thyroid nodules or cyst, deep vein thrombosis.
Elevated white blood cell count, ESR and CRP levels may be seen in the laboratory findings of AST as in our patient. Patients are usually euthyroid, but may rarely develop temporary or permanent hypothyroidism or thyrotoxicosis due to destruction of the gland.(22. Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003; 348(26):2646-55. Review. Erratum in: N Engl J Med. 2003;349(6):620.)Permanent hypothyroidism may occur if the widespread destruction of the gland takes place.(44. Paes JE, Burman KD, Cohen J, Franklyn J, McHenry CR, Shoham S, et al. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid. 2010;20(3):247-55. Review.,66. Türkiye Endokrin ve Metabolizma Hastalıkları Derneği. Tiroid Çalışma Grubu Tiroid Hastalıkları Tanı ve Tedavi Klavuzu 2017. Tiroiditler. Ortadoğu Yayıncılık. 2017; p. 89-103.) There is a tendency for euthyroidism in bacterial infections. While most of the patients with bacterial infections are euthyroid, hypothyroidism in fungal infections and hyperthyroidism in mycobacterial infections are more frequent.(11. Al-Dajani N, Wootton SH. Cervical lymphadenitis, suppurative parotitis, thyroiditis, and infected cysts. Infect Dis Clin North Am. 2007;21(2):523-41, viii. Review.,77. Yu EH, Ko WC, Chuang YC, Wu TJ. Suppurative Acinetobacter baumanii thyroiditis with bacteremic pneumonia: case report and review. Clin Infect Dis. 1998;27(5):1286-90. Review.)
Staphylococcus and Streptococcus are the most common pathogens in AST (about 40%), and Gram-negative agents take the second place (25%).(77. Yu EH, Ko WC, Chuang YC, Wu TJ. Suppurative Acinetobacter baumanii thyroiditis with bacteremic pneumonia: case report and review. Clin Infect Dis. 1998;27(5):1286-90. Review.,88. Yedla N, Pirela D, Manzano A, Tuda C, Lo Presti S. Thyroid Abscess: Challenges in Diagnosis and Management. J Investig Med High Impact Case Rep. 2018;6:2324709618778709.)Methicillin-resistant Staphylococcus aureus-identified cases are also present.(99. Lethert K, Bowerman J, Pont A, Earle K, Garcia-Kennedy R. Methicillin-resistant Staphylococcus aureus suppurative thyroiditis with thyrotoxicosis. Am J Med. 2006;119(11):e1-2.) Acute suppurative thyroiditis is also caused by mycobacterial infections.(77. Yu EH, Ko WC, Chuang YC, Wu TJ. Suppurative Acinetobacter baumanii thyroiditis with bacteremic pneumonia: case report and review. Clin Infect Dis. 1998;27(5):1286-90. Review.)E. corrodens is a fastidious, facultative anaerobic Gram-negative bacillus, which is found in the gastrointestinal and oral flora, and catalase negative, oxidase positive, urease negative, indole negative. These bacteria can survive in aerobic and anaerobic environments, but cause slow-course infections. They are generally susceptible to ampicillin, chloramphenicol, and tetracycline.(1010. Lacroix JM, Walker C. Characterization of a beta-lactamase found in Eikenella corrodens. Antimicrob Agents Chemother. 1991;35(5):886-91.)
Empirical antibiotic therapy in AST should be started without waiting for the results of the culture. The treatment may be only antibiotic therapy in AST or antibiotic treatment after surgical drainage in the presence of abscess. There are some reports of treatment of abscess with aspiration drainage instead of surgical drainage.(1111. Ilyin A, Zhelonkina N, Severskaya N, Romanko S. Nonsurgical management of thyroid abscess with sonographically guided fine needle aspiration. J Clin Ultrasound. 2007;35(6):333-7.) Surgery should be preferred in the presence of fistula or anatomical problems.(22. Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003; 348(26):2646-55. Review. Erratum in: N Engl J Med. 2003;349(6):620.,33. Pereira KD, Losh GG, Oliver D, Poole MD. Management of anomalies of the third and fourth branchial pouches. Int J Pediatr Otorhinolaryngol. 2004; 68(1):43-50.)Thyroidectomy can be performed in patients who were presented with diffuse infiltrative, multiple abscess and who have progression of the disease despite antibiotic therapy.(22. Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003; 348(26):2646-55. Review. Erratum in: N Engl J Med. 2003;349(6):620.) Of course, when planning surgical treatment, etiologic factors should be considered. Fistula resection or brachial cyst excision may be added to surgery in patients with pyriform sinus fistula.(33. Pereira KD, Losh GG, Oliver D, Poole MD. Management of anomalies of the third and fourth branchial pouches. Int J Pediatr Otorhinolaryngol. 2004; 68(1):43-50.,44. Paes JE, Burman KD, Cohen J, Franklyn J, McHenry CR, Shoham S, et al. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid. 2010;20(3):247-55. Review.)In our case, FNAB was performed instead of incisional drainage, due to multiple millimetric abscess foci. Symptomatic and antithyroid drugs were given to reduce the effects of thyrotoxicosis. Antibiotherapy was applied for infection and abscess control.
CONCLUSION
We reported our diagnosis and treatment approach to a case of spontaneous acute suppurative thyroiditis, which is a very rare disease, accompanied by thyrotoxicosis and caused by Eikenella corrodens. It should be kept in mind that, acute suppurative thyroiditis may develop spontaneously with findings of thyrotoxicosis, even with no risk factors. Symptoms of acute suppurative thyroiditis accompanied by thyrotoxicosis may be serious and life-threatening. This potentially fatal picture must be quickly diagnosed, and treatment should be initiated immediately.
REFERENCES
-
1Al-Dajani N, Wootton SH. Cervical lymphadenitis, suppurative parotitis, thyroiditis, and infected cysts. Infect Dis Clin North Am. 2007;21(2):523-41, viii. Review.
-
2Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003; 348(26):2646-55. Review. Erratum in: N Engl J Med. 2003;349(6):620.
-
3Pereira KD, Losh GG, Oliver D, Poole MD. Management of anomalies of the third and fourth branchial pouches. Int J Pediatr Otorhinolaryngol. 2004; 68(1):43-50.
-
4Paes JE, Burman KD, Cohen J, Franklyn J, McHenry CR, Shoham S, et al. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid. 2010;20(3):247-55. Review.
-
5Kondo T. Acute suppurative thyroiditis secondary to pyriform sinus fistula. Lancet Infect Dis. 2019;19(4):447.
-
6Türkiye Endokrin ve Metabolizma Hastalıkları Derneği. Tiroid Çalışma Grubu Tiroid Hastalıkları Tanı ve Tedavi Klavuzu 2017. Tiroiditler. Ortadoğu Yayıncılık. 2017; p. 89-103.
-
7Yu EH, Ko WC, Chuang YC, Wu TJ. Suppurative Acinetobacter baumanii thyroiditis with bacteremic pneumonia: case report and review. Clin Infect Dis. 1998;27(5):1286-90. Review.
-
8Yedla N, Pirela D, Manzano A, Tuda C, Lo Presti S. Thyroid Abscess: Challenges in Diagnosis and Management. J Investig Med High Impact Case Rep. 2018;6:2324709618778709.
-
9Lethert K, Bowerman J, Pont A, Earle K, Garcia-Kennedy R. Methicillin-resistant Staphylococcus aureus suppurative thyroiditis with thyrotoxicosis. Am J Med. 2006;119(11):e1-2.
-
10Lacroix JM, Walker C. Characterization of a beta-lactamase found in Eikenella corrodens. Antimicrob Agents Chemother. 1991;35(5):886-91.
-
11Ilyin A, Zhelonkina N, Severskaya N, Romanko S. Nonsurgical management of thyroid abscess with sonographically guided fine needle aspiration. J Clin Ultrasound. 2007;35(6):333-7.
Publication Dates
-
Publication in this collection
23 Mar 2020 -
Date of issue
2020
History
-
Received
12 July 2019 -
Accepted
27 Nov 2019