Abstract
Objective to create an educational material for preschool teachers to middle school teachers regarding the needed behavior and care to be done during a daily basis towards children living with type 1 Diabetes Mellitus.
Method descriptive exploratory study conducted in five stages: exploratory research, selection of topics to be addressed in the video, literature research on the selected topics, script production and video development. Topics with a knowledge deficit greater than 70% were included and visual techniques were used that increase cognitive load and engagement.
Results 4 articles were chosen, analyzed, and the selected topics were incorporated. The produced video addresses the main knowledge deficits about Type 1 Diabetes among teachers, based on reliable diabetes guidelines.
Conclusion and implication for practice the video proves to be an easily accessible tool, quick to watch, facilitating its use. Thus, it is concluded that the material resulting from this study serves as a facilitator for diabetes education in schools.
Keywords:
Diabetes Mellitus, Type 1; Faculty; Health Education; Instructional Film and Video; Knowledge
Resumo
Objetivo elaborar um vídeo educativo para professores do Ensino Infantil e Fundamental sobre os cuidados e condutas que precisam ser tomadas durante o dia a dia escolar de crianças com Diabetes Mellitus Tipo 1 (DM1).
Método estudo descritivo exploratório realizado em cinco etapas: pesquisa exploratória, seleção dos tópicos a serem abordados no vídeo, pesquisa na literatura sobre os tópicos selecionados, produção do roteiro e elaboração do vídeo. Foram incluídos os tópicos com déficit de conhecimento maior que 70% e utilizadas as técnicas visuais que aumentam a carga cognitiva e o engajamento.
Resultados elegeram-se quatro artigos, os quais foram analisados, e os tópicos selecionados. O vídeo produzido aborda os principais déficits de conhecimento dos professores em relação ao DM1 e apresenta informações oriundas de diretrizes médicas confiáveis sobre a DM.
Conclusão e implicação para prática o vídeo demonstra ser uma ferramenta de fácil acesso, de rápida visualização, facilitando a sua utilização e aplicação. Com isso, conclui-se que o material resultante deste estudo se mostra como um facilitador da educação em DM nas escolas.
Palavras-chave:
Conhecimento; Diabetes Mellitus Tipo 1; Educação em Saúde; Filme e Vídeo Educativo; Professores
Resumen
Objetivo desarrollar un video educativo para maestros de jardín de infantes y escuela primaria sobre el cuidado y los comportamientos requeridos durante la vida escolar diaria de niños con Diabetes Mellitus Tipo 1 (DMT1).
Método este estudio descriptivo y exploratorio se realizó en cinco etapas: investigación exploratoria, selección de temas a ser cubiertos en el video, búsqueda bibliográfica sobre los temas seleccionados, producción de guion y producción de video. Se incluyeron temas con un déficit de conocimiento superior al 70% y se utilizaron técnicas visuales que aumentan la carga cognitiva y el compromiso.
Resultados se seleccionaron y analizaron cuatro artículos y se seleccionaron los temas. El video aborda los principales déficits de conocimiento de los maestros con respecto a la DMT1 y presenta información de guías médicas confiables sobre la DMT1.
Conclusión e implicaciones para la práctica El video demuestra ser una herramienta de fácil acceso y rápida visualización, facilitando su uso y aplicación. Por lo tanto, concluimos que el material resultante de este estudio puede facilitar la educación sobre la DM en las escuelas.
Palabras clave:
Conocimiento; Diabetes Mellitus Tipo 1; Docentes; Educación en Salud; Películas y Videos Educativos
INTRODUCTION
Diabetes mellitus (DM) is a metabolic disorder characterized by persistent hyperglycemia resulting from a deficiency in insulin production or action, or both mechanisms.1 DM is considered one of the main public health challenges because, unlike other chronic conditions, it has affected an increasing number of people of working age, leading to a decline in quality of life and an increase in premature deaths, in addition to high costs for control and treatment.2
DM can be classified according to its etiopathogenesis, including Type 1 Diabetes Mellitus (DM1) and Type 2 Diabetes Mellitus (DM2). DM2 is the most common type in the general population, associated with obesity and aging. It is caused by insulin resistance, partial deficiency of insulin secretion by beta cells, and changes in incretin secretion.3 DM1, on the other hand, is a complex disease involving a combination of factors, such as genetic susceptibility, immune dysregulation, and exposure to environmental triggers.4 It is characterized by the destruction of pancreatic beta cells, which produce insulin, through an autoimmune response. When approximately 90% of the cells are destroyed, DM1 becomes clinically symptomatic.5
DM1 can be diagnosed at any age and is the most common type of DM in children and adolescents.6 Its manifestation is acute, with obvious signs and symptoms characteristic of hyperglycemia, such as polyuria, polydipsia, nocturia, enuresis, and weight loss, which may be accompanied by polyphagia, behavioral disorders, decline in school performance, and blurred vision.4
Glycemic control in people with DM1 involves constant glucose monitoring, dietary planning and changes, physical exercise, and insulin administration.7 Adding to this the fact that preschool students spend an average of six hours a day at school, while elementary school students spend five hours a day,8 it is essential that the entire school staff know how to recognize the symptoms and know how to act in cases of both hypoglycemia and hyperglycemia.9
However, several studies on school staff knowledge of DM1 show that there is a knowledge gap on the subject.9-13 During school hours, staff are responsible for the safety and care of students, so it is extremely important that they are trained to provide support in cases of hypoglycemia or hyperglycemia, in addition to assisting with glycemic monitoring and insulin administration.14 A trained and qualified school staff can prevent immediate and late complications caused by these glycemic changes.15
The perception of families of children with DM1 is that most schools do not have the structure or technical preparation to receive these students. According to them, “there is a lack of knowledge among teachers on the subject, a lack of appropriate places for insulin administration, inadequate school meals, and the absence of a nurse or health professional qualified to care for students with special needs.”16:6 While it is difficult for parents and students to trust that school staff will know how to deal with DM, professionals who lack experience are often frightened by the responsibility of caring for a student with DM.14
The level of knowledge about DM1 and the confidence of school educators in dealing with students with the disease, before and after an education program, increased significantly, as pointed out by the results of a quasi-experimental study.17 Given the facts presented, the production and availability of educational materials on the management of children with DM1, intended for education professionals, are extremely important to reduce the risks of both hypoglycemia and hyperglycemia, enabling teachers to act correctly in the face of possible adversities.
For this reason, the objective of this study was to develop an educational video for preschool and elementary school teachers on the care and conduct that should be adopted in the daily school life of children with DM1.
METHOD
The methodological approach was exploratory, qualitative, and descriptive. The study was conducted at the Universidade de Brasília, Faculty of Ceilândia (UnB/FCE), through the creation of an educational video aimed at schoolteachers on the care and conduct of children with DM1, which, according to the literature review, are less known to these professionals.
The video was produced in the following stages: a) exploratory research; b) selection of topics to be addressed in the video; c) literature review on the selected topics; d) production of the script; e) production of the educational video.
Initially, a literature review was conducted to identify studies measuring the level of knowledge of education professionals about DM1. Searches were performed in PubMed/MEDLINE, the Virtual Health Library (VHL), and the CAPES Journal Portal. The Health Sciences Descriptors/Medical Subject Headings (DeCS/MeSH) and Boolean operators were used, generating the following search strategies: a) “School teacher” OR ‘teacher’ AND “Diabetes Mellitus, Type 1” AND “Knowledge”; b) “professor” OR ‘school’ AND “Diabetes Mellitus” AND “knowledge.” The presence of terms in both English and Portuguese in the search strategies is justified by the variety of databases used (PubMed/MEDLINE for international literature and BVS [Virtual Health Library Brazil - VHL] for national literature).
The inclusion criteria were quantitative studies on knowledge of DM1 among education professionals, available in English, Portuguese, or Spanish, with access to the full text. Studies conducted outside Brazil were excluded, as this product is aimed at Brazilian education professionals.
After selecting the studies, the articles were analyzed to identify topics related to DM. Based on this analysis, the percentage of error associated with each topic presented was placed in a table. When more than one study researched the same topic, the arithmetic mean was calculated.
Topics with a deficit of over 70% were selected for inclusion in the video. This percentage was chosen to produce a shorter video, since, according to the literature,18 the average maximum engagement time for a video is six minutes, with short videos, between zero and three minutes, showing less variation in engagement.
After selecting the topics to be addressed in the video, to develop a script with scientifically based information, a search was conducted on the topics in the guidelines of the following medical societies: Brazilian Diabetes Society (SBD),1,3,19,20 International Society for Pediatric and Adolescent Diabetes (ISPAD)21,22 , and International Diabetes Federation (IDF).6
The video was created in a 2D animation format. The illustrations used were created in Adobe IllustratorⓇ and animated in Adobe AnimateⓇ. Adobe IllustratorⓇ is a graphic design tool that allows the creation of illustrations with professional precision.23 Adobe AnimateⓇ enables the creation of frame-by-frame animations.24
These tools were chosen because there is integration between AdobeⓇ software programs, which facilitates the processing of content from creation to editing, since the software can share and edit the same files simultaneously. In addition, the authors are already familiar with these programs.
The video narration was generated using Artificial Intelligence (AI) via the Eleven Labs website. This choice was made to ensure clear audio, without noise or interference from ambient sounds. Finally, in terms of the video's structure, it was produced considering the principles and guidelines for enhancing learning through videos.18 To increase the cognitive load, important information was highlighted using keywords marked by changes in color, size, position, and indicative arrows. To increase engagement, accessible language and narration with more expressive intonation were adopted.
The project did not need to be submitted to the Human Research Ethics Committee (REC), under Resolution No. 466/12 of the National Health Council (NHC), as it was the production of an educational video, based on bibliographic research, without the direct participation of human beings, which does not require the approval of an ethics committee.
RESULTS
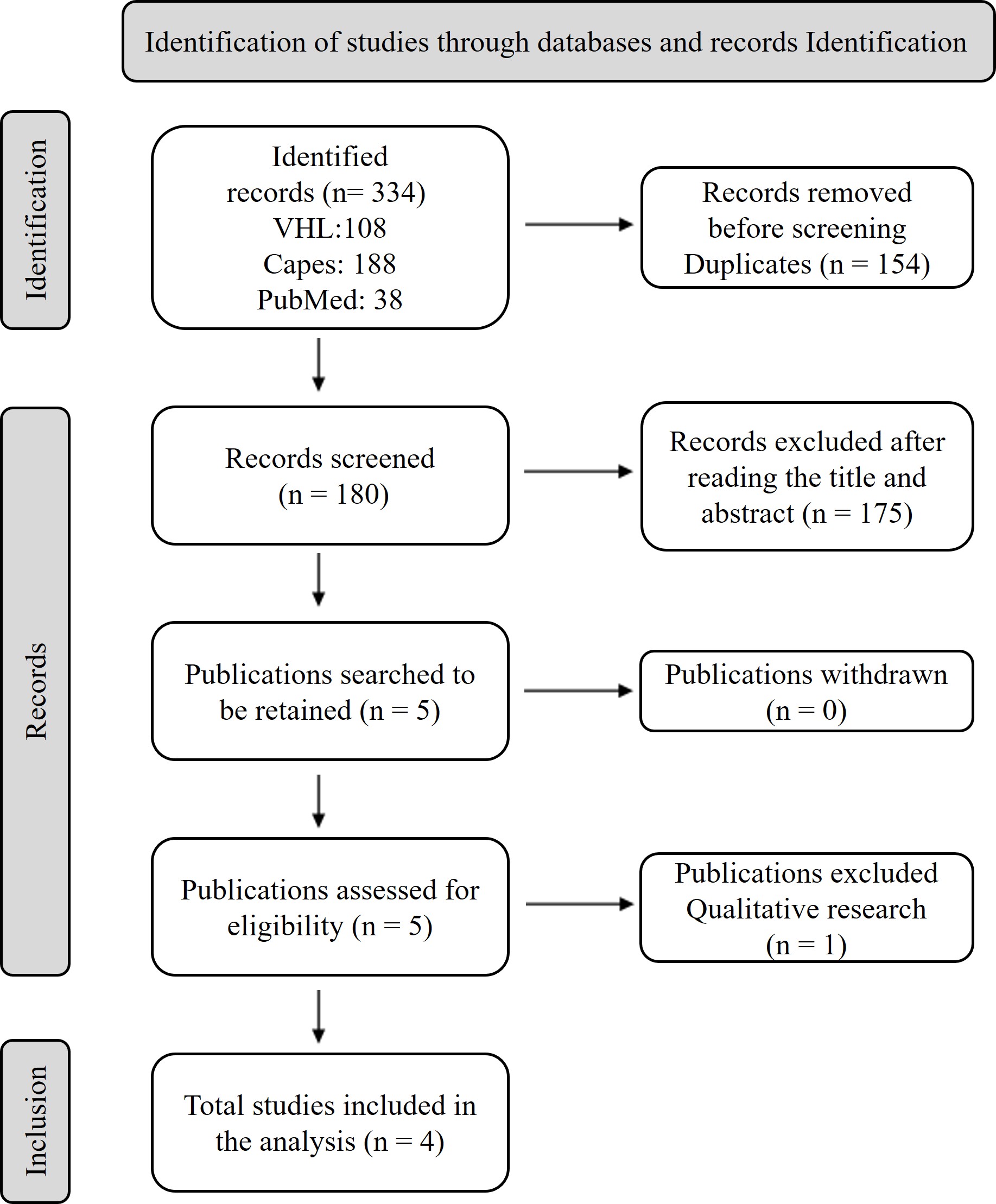
The exploratory research resulted in 334 articles. Of these, 154 were duplicates and 175 were excluded after reading the title and abstract because they did not meet the inclusion criteria. Of the five remaining articles, one was excluded because it was a qualitative research study. In the end, four quantitative articles were analyzed, all of national origin. The research process is described in the flow diagram shown in Figure 1.
The topics identified in the analysis of the selected articles are shown in Table 1. Those with a deficit greater than 70% were: classification of DM, management of hypoglycemia, causes of hypoglycemia, recommendations for better glycemic control, frequency of glycemic monitoring, normal glucose value, fasting blood glucose value for diagnosis, glycemic monitoring during exercise, and diagnostic testing.
Percentage of error and average for each topic studied in the selected articles. Brasília (DF), Brazil, 2023.
Unlike the others, the study conducted in Natal, Rio Grande do Norte, Brazil,13 classified the answers as correct, partially correct, incorrect, and “don’t know.” Table 1 was prepared based on the sum of the percentages of partially correct, incorrect, and “don’t know” answers. Despite this, the percentage referring to the topic “necessary care” was presented by the study with the combination of correct and partially correct answers. Therefore, in Table 1, this topic was the only one in which the error percentage did not consider partially correct answers. The same study investigated knowledge about complications related to DM, but only presented the frequency of responses for each complication, without directly reporting the percentage of complete responses, which is why this topic was not included in Table 1.13
It is worth noting that all topics with a percentage greater than 70% were included in the video. Topics with percentages below 70% may or may not have been mentioned, depending on the need for explanation to improve understanding of the video.
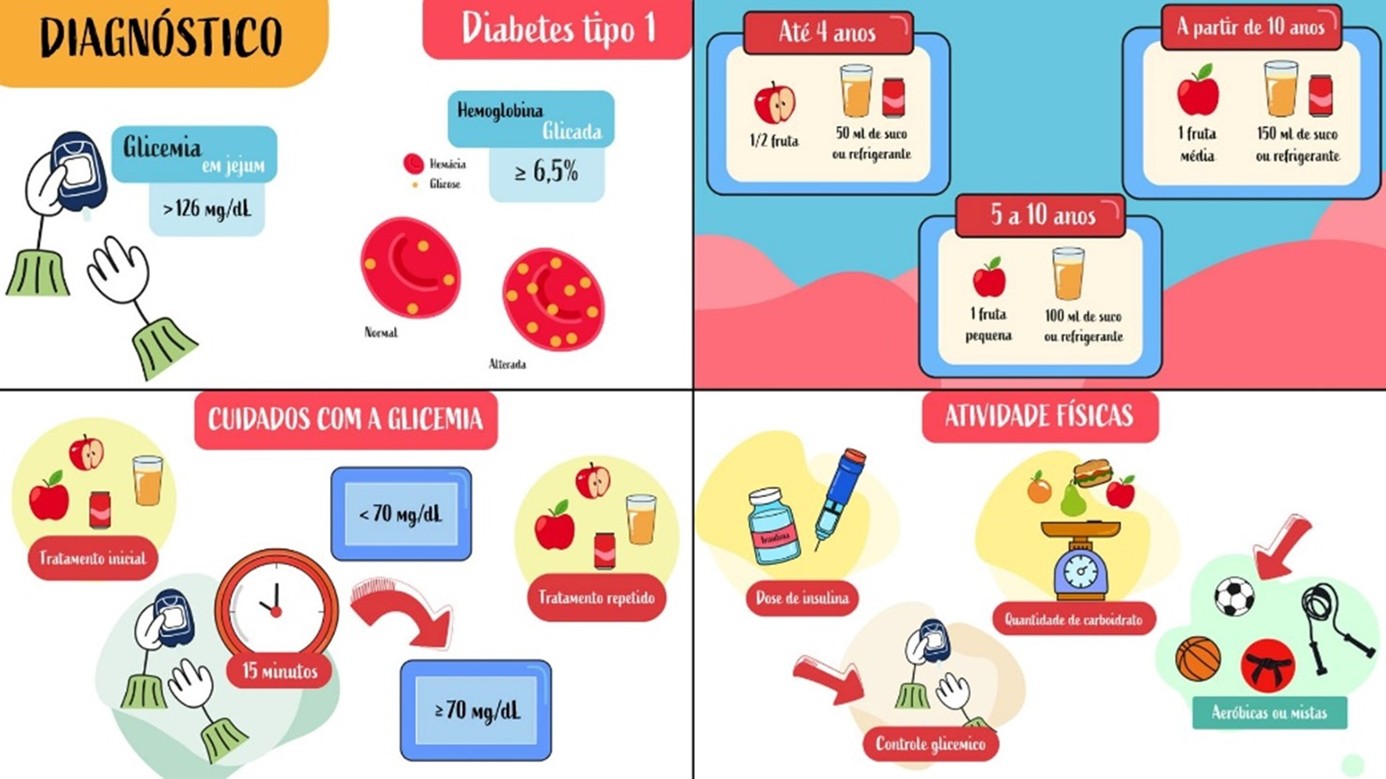
The video produced in portuguese, illustrated in Figure 2, is five minutes and 30 seconds long and can be divided into three main parts: general information about DM, hypoglycemia management, and blood glucose control during exercise. It is available at the following link: https://youtu.be/dyR3C7P2VCE.
DISCUSSION
Despite the selection of only eight topics, it is clear that there is a general lack of knowledge about DM1 among Brazilian education professionals, as 62.5% of the topics had knowledge gaps equal to or greater than 50%. These data corroborate several other studies from different countries, which showed that schoolteachers’ knowledge about DM1 is inadequate.25-28
DM1 has a higher incidence in the 5-15 age group,29 and is caused by the destruction of beta cells, which leads to severe insulin deficiency and, consequently, the need for full insulin therapy as treatment.3 Lack of understanding about the causes and classification of DM contributes to stereotypes and misperceptions about the disease, which can hinder treatment, affect the child's psychological state, and cause embarrassing situations.
The stigma most commonly reported by people with DM in a study conducted in the United States30 was that DM was the result of a failure of personal responsibility, causing patients to feel judged and blamed for the view that the reason they had DM was because they ate too much, did not exercise, were lazy, or were overweight or obese.
A qualitative study31 related to the perception of children with DM1 about the school environment collected reports from teachers who did not allow children to eat during episodes of hypoglycemia, prohibited them from leaving the classroom, and caused embarrassment on festive occasions due to dietary restrictions. There is even a report of a situation in which a child suffered a seizure due to severe hypoglycemia and waited for the mother to arrive because the teacher did not know how to act.31 Given this, it is possible to see that teachers' knowledge about DM can directly influence the glycemic regulation of children with DM1.
A study identified a relationship between school staff training and reduced levels of glycated hemoglobin (HbA1c) in children.32 HbA1c is hemoglobin A that undergoes glycation at a terminal valine in the beta chain and is used as an indicator of the average blood sugar level throughout the life of erythrocytes. Hemoglobin A1c monitoring is considered a gold standard test because it allows for the estimation of blood glucose levels over the past three to four months.33 The results of the study indicated that children enrolled in schools whose staff had been trained had significantly lower HbA1c levels.32 In addition, indirect evidence suggested that residents of countries with structured education programs had better glycemic control.34
A study investigating the level of knowledge about DM1 among physical education teachers concluded that most participants did not know in which situations physical exercise was contraindicated. In addition, 81% of teachers did not perform capillary blood glucose testing, and among the 19% who did, only 3.4% performed the measurement before and after physical exercise—considered the ideal procedure.10
Aerobic physical exercise tends to cause a rapid drop in blood glucose, while anaerobic and mixed forms of exercise may be associated with a smaller drop or even an increase in blood glucose.22 During light and moderate physical exercise, insulin sensitivity is increased by stimulating glucose uptake by the muscle, which can lead to episodes of hypoglycemia; while high-intensity exercise stimulates glucose production by the liver and can lead to hyperglycemia.35 To circumvent these effects, constant monitoring of blood glucose, carbohydrate intake, and insulin administration is recommended, with the latter two always dependent on glucose levels and the type of exercise being performed.19
These physiological effects and the care they require make knowledge about the frequency of glycemic monitoring, procedures in case of hypoglycemia, and reasoning about carbohydrate intake, depending on the type of exercise, included in the video produced, indispensable for physical education teachers.
Younger children with DM1 tend to have more frequent episodes of hypoglycemia because they exercise more and consume less food, in addition to having a decrease in counterregulatory hormonal responses to hypoglycemia through autonomic function.36 During these moments, it is important that there be immediate intervention so that mild or moderate hypoglycemia does not progress to severe hypoglycemia.37 And it is for this reason that knowledge about the management of hypoglycemia by education professionals is necessary.
The treatment of DM1 is based on the triad of insulin use, physical exercise, and proper nutrition.1 However, only one article questioned the medication used for glycemic control, and none researched knowledge about how to administer insulin. For this reason, no information about insulin was included in the video, which represents a limitation of this study.
Although there is no information about insulin in the video, it should be kept in mind that young children are not independent in making decisions about DM, and when school support is limited, these children may receive an insufficient amount of insulin.37 Therefore, it is important that education professionals be better informed about insulin administration.
In the context of using videos as a teaching strategy, it has been observed that it enhances the learning process by stimulating both the visual and auditory channels, providing multiple approaches to understanding the content.38 A systematic review showed that educational videos about DM, aimed at patients themselves, promoted improved care, knowledge, and self-care, decreased HbA1C, and increased attendance at complementary exams.39 In another study, an improvement in educators' knowledge and confidence in the management of DM1 was observed, demonstrating the effectiveness of educational programs and reinforcing the need for educational interventions.17
The Kids & Diabetes in Schools (KiDS) project, created by the IDF in conjunction with ISPAD and Sanofi Diabetes, has developed a series of educational materials for school teachers, parents of children with DM, parents of children without DM, and children without DM themselves. Brazil and India were selected as pilot countries for the dissemination of this material, with training sessions for teachers and the provision of printed material for children and their parents in 15 schools in each country. The implementation of this project had a positive impact on staff confidence and the school experience of children with DM1.40
The eight videos produced by the project are available on the SBD official website. Each video discusses a different topic related to DM, generating 39 minutes and 28 seconds of content in total. The video in this study differs from the existing content in this project in that it addresses the main content deficits identified by Brazilian education professionals, presenting more succinct and quickly accessible content.
This study innovates by integrating national quantitative data on gaps in teacher knowledge into a digital educational product adapted to the average engagement time, which increases the potential for educational impact in Brazilian schools. Future research may evaluate the effectiveness of the video in real school contexts and explore its adaptation to other chronic conditions in childhood.
CONCLUSION AND IMPLICATIONS FOR PRACTICE
The video produced is an easily accessible and quick-to-view tool, making it ideal for use by education professionals. However, this study has some limitations that should be considered. The first relates to the selection of topics covered, which is limited to knowledge deficits greater than 70%, which reinforces the quality of the selected articles, but consequently excludes some relevant information, such as insulin administration.
Another limitation is related to the practical applicability of the content in schools, since the availability of resources, such as glucometers, test strips, and blood ketone monitors, may vary among educational institutions, compromising the implementation of the suggested behaviors. In addition, the small number of articles included in the review and the lack of standardization in the categorization of responses in the studies analyzed may have influenced the selection of topics covered, limiting the scope of the material produced.
Given the positive impact that educational materials on health can have on society, further studies are needed to develop more dynamic, clear, and objective educational tools on relevant public health topics.
Thus, based on the video production process and previous research highlighting the benefits of DM education, it can be concluded that the material developed is a resource with the potential to facilitate the dissemination of knowledge about the management of Type 1 Diabetes Mellitus in the school environment. In addition, it can contribute to clinical practice by providing relevant and applicable information on the topic, applicable at different levels of health care, covering actions ranging from prevention to intervention, treatment, and rehabilitation.
It is recommended that the video development and evaluation model be replicated in different educational contexts and with other health topics, expanding the scope of health education in schools. In addition, there is a need to validate the video in future studies, with the active participation of teachers—the main target audience for this technology—to verify its applicability, acceptability, and effectiveness. It is also suggested that the impact of the video as an educational tool be measured, considering its possible adaptation for other audiences, such as family members and caregivers, which could expand its potential reach and contribution to health care.
ACKNOWLEDGEMENTS
No acknowledgments.
DATA AVAILABILITY RESEARCH
The contents underlying the research text are included in the article.
-
a
Extracted from the undergraduate thesis: “Production of an educational video on Type 1 Diabetes Mellitus in children for education professionals,” presented to the Physical Therapy Course at the Faculty of Health Sciences and Technologies, Universidade de Brasília, in 2023.
-
FINANCIAL SUPPORT
No funding.
References
-
1 Sociedade Brasileira de Diabetes. Diretrizes Sociedade Brasileira de Diabetes 2019-2020 [Internet]. São Paulo: SBD; 2019 [citado 2023 out 5]. Disponível em: https://www.saude.ba.gov.br/wp-content/uploads/2020/02/Diretrizes-Sociedade-Brasileira-de-Diabetes-2019-2020.pdf
» https://www.saude.ba.gov.br/wp-content/uploads/2020/02/Diretrizes-Sociedade-Brasileira-de-Diabetes-2019-2020.pdf -
2 Ministério da Saúde (BR). Boletim Epidemiológico [Internet]. Vol. 53. Brasília: Ministério da Saúde; 2022 [citado 2023 jan 5]. Disponível em: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/boletins/epidemiologicos/edicoes/2022/boletim-epidemiologico-vol-53-no45/view
» https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/boletins/epidemiologicos/edicoes/2022/boletim-epidemiologico-vol-53-no45/view -
3 Rodacki M, Teles M, Gabbay M, Montenegro R, Bertoluci M. Classificação do diabetes. In: Montenegro R, Bertoluci M, editores. Diretriz Oficial da Sociedade Brasileira de Diabetes. São Paulo: SBD; 2022. http://doi.org/10.29327/557753.2022-1
» http://doi.org/10.29327/557753.2022-1 -
4 Acharjee S, Ghosh B, Al-Dhubiab BE, Nair AB. Understanding Type 1 Diabetes: etiology and models. Can J Diabetes. 2013 ago 1;37(4):269-76. http://doi.org/10.1016/j.jcjd.2013.05.001 PMid:24070892.
» http://doi.org/10.1016/j.jcjd.2013.05.001 -
5 Mayer-Davis EJ, Kahkoska AR, Jefferies C, Dabelea D, Balde N, Gong CX et al. ISPAD Clinical Practice Consensus Guidelines 2018: definition, epidemiology, and classification of diabetes in children and adolescents. Pediatr Diabetes. 2018;19(Suppl 27):7-19. http://doi.org/10.1111/pedi.12773 PMid:30226024.
» http://doi.org/10.1111/pedi.12773 -
6 International Diabetes Federation. IDF Diabetes Atlas [Internet]. 10th ed. Brussels: IDF; 2021 [citado 2023 jan 9]. 141 p. Disponível em: https://diabetesatlas.org/atlas/tenth-edition/
» https://diabetesatlas.org/atlas/tenth-edition/ -
7 Lawrence SE, Cummings EA, Pacaud D, Lynk A, Metzger DL. Managing type 1 diabetes in school: Recommendations for policy and practice. Paediatr Child Health. 2015;20(1):35-44. http://doi.org/10.1093/pch/20.1.35 PMid:25722642.
» http://doi.org/10.1093/pch/20.1.35 -
8 Instituto Nacional de Estudos e Pesquisas Educacionais Anísio Teixeira. Média de Horas-aula diária [Internet]. Brasília: INEP; 2022 [citado 2023 out 5]. Disponível em: https://www.gov.br/inep/pt-br/acesso-a-informacao/dados-abertos/indicadores-educacionais/media-de-horas-aula-diaria
» https://www.gov.br/inep/pt-br/acesso-a-informacao/dados-abertos/indicadores-educacionais/media-de-horas-aula-diaria -
9 Camargo LC, Carvalho D. Conhecimentos da equipe escolar sobre diabetes mellitus tipo 1. Rev Ibero-Am Estud Educ. 2020;15(2):619-30. https://doi.org/10.21723/riaee.v15i2.13327
» https://doi.org/10.21723/riaee.v15i2.13327 -
10 Monteiro LZ, Spinato IL, Pinheiro MHNP, Silva CAB, Montenegro RM Jr. Exercicio Fisico em Crianças com Diabetes Mellitus Tipo 1: conhecimento do Profissional de Educação Fisica. Rev Bras Ciênc Mov. 2009;17(2):1-23. https://doi.org/10.18511/rbcm.v17i2.897
» https://doi.org/10.18511/rbcm.v17i2.897 - 11 Nass EMA, Reis P, Teston EF, Ichisato SMT, Salci MA, Marcon SS. Knowledge of teachers of elementary school on diabetes and its management in the school environment. REME - Rev Min Enferm. 2019;23:e-1186. https://doi.org/10.5935/1415-2762.20190034.
-
12 Simões AL, Stacciarin TS, Dal Poggetto MT, Maruxo HB, Soares HM, Simões ACA. Conhecimento dos professores sobre o manejo da criança com diabetes mellitus. Texto Contexto Enferm. 2010;19(4):651-7. http://doi.org/10.1590/S0104-07072010000400007
» http://doi.org/10.1590/S0104-07072010000400007 -
13 Garcia RS, Araújo DVG, Silva GO, Medeiros GSD, Barros SS, Garcia CS. Conhecimento sobre diabetes mellitus entre profissionais da rede pública de ensino. Rev Bras Promoc Saude. 2017;30(1):57-63. http://doi.org/10.5020/18061230.2017.p57
» http://doi.org/10.5020/18061230.2017.p57 -
14 Lawrence SE, Albanese‐O’Neill A, Besançon S, Black T, Bratina N, Chaney D et al. Clinical Practice Consensus Guidelines 2022: management and support of children and adolescents with diabetes in school. Pediatr Diabetes. 2022;23(8):1478-95. http://doi.org/10.1111/pedi.13432 PMid:36537526.
» http://doi.org/10.1111/pedi.13432 -
15 Jackson CC, Albanese-O’Neill A, Butler KL, Chiang JL, Deeb LC, Hathaway K et al. Diabetes care in the school setting: a position statement of the American Diabetes Association. Diabetes Care. 2015;38(10):1958-63. http://doi.org/10.2337/dc15-1418 PMid:26404925.
» http://doi.org/10.2337/dc15-1418 -
16 Gonçalves CBCD, Mantovani RM, Albuquerque CTM, Reis JS, Gomes VMR. O aluno com diabetes: avaliação dos pais sobre o ambiente escolar. Rev Med Minas Gerais [citado 2025 abr 7]. 2022 [Internet]. 32:32112. Disponível em: https://rmmg.org/artigo/detalhes/3924
» https://rmmg.org/artigo/detalhes/3924 -
17 Dixe MACR, Gordo CMGO, Catarino HBP, Kraus T, Menino EPSG. Effects of an education program on knowledge and self-perception of school personnel in preparing to care for type 1 diabetes students. Einstein (Sao Paulo). 2020;18:eAO5101. http://doi.org/10.31744/einstein_journal/2020AO5101 PMid:32130327.
» http://doi.org/10.31744/einstein_journal/2020AO5101 -
18 Brame CJ. Effective educational videos: principles and guidelines for maximizing student learning from video content. CBE Life Sci Educ. 2016;15(4):es6. http://doi.org/10.1187/cbe.16-03-0125 PMid:27789532.
» http://doi.org/10.1187/cbe.16-03-0125 -
19 Pereira WVC, Vancea DMM, Oliveira RA, de Freitas YGPC, Lamounier DrRN, Zagury RL. Atividade física e exercício no DM1. In: Bertoluci M, editor. Diretriz Oficial da Sociedade Brasileira de Diabetes [Internet]. São Paulo: SBD; 2022 [citado 2023 jan 11]. Disponível em: https://diretriz.diabetes.org.br/atividade-fisica-e-exercicio-fisico-no-diabetes-mellitus-tipo-1/
» https://diretriz.diabetes.org.br/atividade-fisica-e-exercicio-fisico-no-diabetes-mellitus-tipo-1/ -
20 Pititto BA, Dias ML, Moura FF, Lamounier R, Vencio S, Calliari LE. Metas no tratamento do diabetes. In: Bertoluci M, editor. Diretriz Oficial da Sociedade Brasileira de Diabetes. São Paulo: SBD; 2022. http://doi.org/10.29327/557753.2022-3
» http://doi.org/10.29327/557753.2022-3 -
21 Abraham MB, Karges B, Dovc K, Naranjo D, Arbelaez AM, Mbogo J et al. ISPAD Clinical Practice Consensus Guidelines 2022: assessment and management of hypoglycemia in children and adolescents with diabetes. Pediatr Diabetes. 2022 dez 20;23(8):1322-40. http://doi.org/10.1111/pedi.13443 PMid:36537534.
» http://doi.org/10.1111/pedi.13443 -
22 Adolfsson P, Taplin CE, Zaharieva DP, Pemberton J, Davis EA, Riddell MC et al. ISPAD Clinical Practice Consensus Guidelines 2022: exercise in children and adolescents with diabetes. Pediatr Diabetes. 2022 dez 20;23(8):1341-72. http://doi.org/10.1111/pedi.13452 PMid:36537529.
» http://doi.org/10.1111/pedi.13452 -
23 ADOBE. Software de desenhos vetoriais líder do setor [Internet]. Adobe Illustrator [citado 2023 jan 16]. Disponível em: https://www.adobe.com/br/products/illustrator.html
» https://www.adobe.com/br/products/illustrator.html -
24 ADOBE. Software de animação 2D e Flash [Internet]. Adobe Animate [citado 2023 jan 16]. Disponível em: https://www.adobe.com/br/products/animate.html
» https://www.adobe.com/br/products/animate.html -
25 Gutiérrez-Manzanedo JV, Carral-San Laureano F, Moreno-Vides P, de Castro-Maqueda G, Fernández-Santos JR, Ponce-González JG. Teachers’ knowledge about type 1 diabetes in south of Spain public schools. Diabetes Res Clin Pract. 2018 set;143:140-5. http://doi.org/10.1016/j.diabres.2018.07.013 PMid:30006308.
» http://doi.org/10.1016/j.diabres.2018.07.013 -
26 Aycan Z, Önder A, Çetinkaya S, Bilgili H, Yıldırım N, Baş VN et al. Assessment of the knowledge of Diabetes Mellitus Among School Teachers within the Scope of the Managing Diabetes at School Program. J Clin Res Pediatr Endocrinol. 2012;4(4):199-203. http://doi.org/10.4274/Jcrpe.756 PMid:23032146.
» http://doi.org/10.4274/Jcrpe.756 -
27 Wright A, Chopak-Foss J. School personnel knowledge and perceived skills in diabetic emergencies in Georgia Public Schools. J Sch Nurs. 2020;36(4):304-12. http://doi.org/10.1177/1059840518820106 PMid:30595093.
» http://doi.org/10.1177/1059840518820106 - 28 Alshammari FM, Haridi HK. Teachers’ knowledge about type 1 diabetes in public female elementary schools in Northern Saudi Arabia. J Prev Med Hyg. 2021 set;62(3):E673-80. PMid:34909495.
-
29 Merino MFGL, Oliveira RR, Silva PLAR, Carvalho MDB, Pelloso SM, Higarashi IH. Hospitalization and mortality by diabetes mellitus in children: analysis of temporal series. Rev Bras Enferm. 2019 dez;72(suppl 3):147-53. http://doi.org/10.1590/0034-7167-2018-0299 PMid:31851247.
» http://doi.org/10.1590/0034-7167-2018-0299 -
30 Liu NF, Brown AS, Folias AE, Younge MF, Guzman SJ, Close KL et al. Stigma in people with Type 1 or Type 2 Diabetes. Clin Diabetes. 2017;35(1):27-34. http://doi.org/10.2337/cd16-0020 PMid:28144043.
» http://doi.org/10.2337/cd16-0020 -
31 Sparapani VC, Liberatore RDR, Damião EBC, Oliveira Dantas IR, Camargo RAA, Nascimento LC. Children with Type 1 Diabetes Mellitus: self‐management experiences in school. J Sch Health. 2017 ago 9;87(8):623-9. http://doi.org/10.1111/josh.12529 PMid:28691177.
» http://doi.org/10.1111/josh.12529 -
32 Wagner J, Heapy A, James A, Abbott G. Brief report: glycemic control, quality of life, and school experiences among students with diabetes. J Pediatr Psychol. 2006 set 1;31(8):764-9. http://doi.org/10.1093/jpepsy/jsj082 PMid:16162839.
» http://doi.org/10.1093/jpepsy/jsj082 -
33 Gabbay MAL, Rodacki M, Calliari LE, Vianna AGD, Krakauer M, Pinto MS et al. Time in range: a new parameter to evaluate blood glucose control in patients with diabetes. Diabetol Metab Syndr. 2020 mar 16;12(1):22. http://doi.org/10.1186/s13098-020-00529-z PMid:32190124.
» http://doi.org/10.1186/s13098-020-00529-z -
34 Lindholm Olinder A, DeAbreu M, Greene S, Haugstvedt A, Lange K, Majaliwa ES et al. ISPAD Clinical Practice Consensus Guidelines 2022: diabetes education in children and adolescents. Pediatr Diabetes. 2022 dez 20;23(8):1229-42. http://doi.org/10.1111/pedi.13418 PMid:36120721.
» http://doi.org/10.1111/pedi.13418 -
35 Codella R, Terruzzi I, Luzi L. Why should people with type 1 diabetes exercise regularly? Acta Diabetol. 2017 jul 14;54(7):615-30. http://doi.org/10.1007/s00592-017-0978-x PMid:28289908.
» http://doi.org/10.1007/s00592-017-0978-x -
36 Urakami T. Severe hypoglycemia: is it still a threat for children and adolescents with Type 1 Diabetes? Front Endocrinol (Lausanne). 2020;11:609. http://doi.org/10.3389/fendo.2020.00609 PMid:33042005.
» http://doi.org/10.3389/fendo.2020.00609 -
37 Lawrence SE, Cummings EA, Pacaud D, Lynk A, Metzger DL. Managing type 1 diabetes in school: recommendations for policy and practice. Paediatr Child Health. 2015;20(1):35-44. http://doi.org/10.1093/pch/20.1.35 PMid:25722642.
» http://doi.org/10.1093/pch/20.1.35 -
38 Stockwell BR, Stockwell MS, Cennamo M, Jiang E. Blended learning improves science education. Cell. 2015;162(5):933-6. http://doi.org/10.1016/j.cell.2015.08.009 PMid:26317458.
» http://doi.org/10.1016/j.cell.2015.08.009 - 39 Hoe CYW, Ahmad B, Watterson J. The use of videos for diabetes patient education: a systematic review. Diabetes Metab Res Rev. 2024;40(2):e3722. PMid:37690072.
-
40 Chinnici D, Middlehurst A, Tandon N, Arora M, Belton A, Reis Franco D et al. Improving the school experience of children with diabetes: evaluation of the KiDS project. J Clin Transl Endocrinol. 2019;15:70-5. http://doi.org/10.1016/j.jcte.2018.12.001 PMid:30792956.
» http://doi.org/10.1016/j.jcte.2018.12.001
Edited by
-
ASSOCIATED EDITOR
Pedro Ricardo Martins Bernardes Lucas https://orcid.org/0000-0002-2560-7306
-
SCIENTIFIC EDITOR
Marcelle Miranda da Silva https://orcid.org/0000-0003-4872-7252
Publication Dates
-
Publication in this collection
22 Sept 2025 -
Date of issue
2025
History
-
Received
07 Apr 2025 -
Accepted
26 June 2025

 Development of an educational video on type 1 diabetes mellitus for primary education professionals
Development of an educational video on type 1 diabetes mellitus for primary education professionals